- What We Treat
- Anxiety
- Depression
- What Is Depression?
- Common Signs of Depression in Teenagers
- Causes of Depression in Teens
- School Resources and Counseling Support for Teen Depression
- Benefits of Residential Treatment for Teens With Depression
- Therapy Options for Teenage Depression
- How to Talk to Your Parents About Getting Help for Depression
- Alternative and Holistic Treatments for Teen Depression
- Medication for Teen Depression
- Healthy Ways to Cope with Depression as a Teen
- Impact of Depression on School, Friendships, and Daily Life
- How Depression Affects the Teenage Brain
- Recognizing Hidden Depression in High-Achieving Teens
- Gender Differences in Teen Depression
- Depression and Anxiety in Teens: What Makes Them Different and How Do They Connect?
- Bipolar Disorder
- Mood And Thought Disorder
- Trauma And PTSD
- ADHD
- Schizophrenia
- Technology Dependence
- Academic & Social Challenges
- Self-Harm
- Psychosis
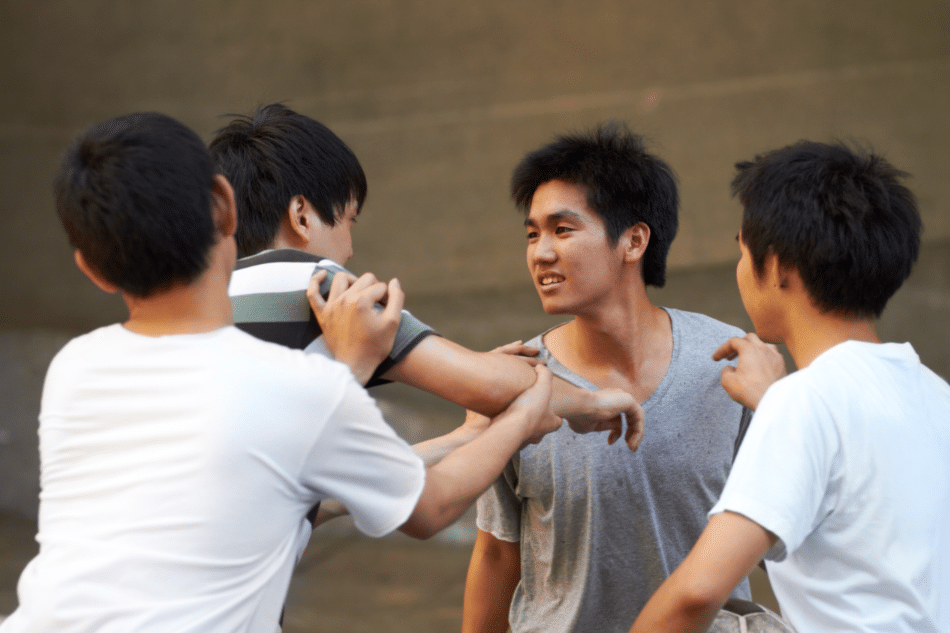
- Anger Treatment
- Trauma and Abuse Treatment
- Mental Health Services
- Locations
- Programs
- Cost
- About Us
- Resources
- Blog
- Resources for Teachers & Community Leaders
- Building a Mental Health Action Plan for Your School
- Recognizing Warning Signs of Teen Mental Illness
- How to Communicate With Families
- How to Identify Early Warning Signs of Mental Illness in Students
- Supporting a Student After Mental Health Leave
- Supporting LGBTQ+ Youth in Crisis
- Implementing School-Based Mental Health Screenings
- Resources for Parents & Caregivers
- Legal Rights for Patients & Families
- Washington State Teen Mental Health Rights
- The Role of Mental Health Tribunals
- Recognizing Mistreatment in Adolescent Mental Health Treatment
- Teen Psychiatric Hospitalization: Voluntary vs. Involuntary Commitment
- Understanding 504 Plans and IEPs for Mental Health Needs
- The Role of Guardianship in Adolescent Mental Health Care
- Teens & Mental Health Rights: Confidentiality & Consent
- Parent’s Guide to Mental Health Support
- What to Do When Your Child Is in a Mental Health Crisis
- How Families Can Be Involved in Residential and Outpatient Care
- Is Residential Treatment Right for Your Teen?
- How to Prepare for Your Child’s Admission to Residential Treatment
- Setting Boundaries When Supporting Someone in Treatment
- Supporting a Child with Severe Mental Illness
- Supporting Your Child in Treatment
- What to Say to Someone in a Mental Health Crisis
- Recognizing Codependency in Teens
- Confidentiality and Mental Health Referrals
- Overcoming Common Barriers to Mental Health Treatment
- Stigma and Guilt Around Seeking Mental Health Care
- Taking Time Off School for Mental Health
- Creating a Plan for When Your Child Returns Home
- How to Mentally Prepare for Leaving Your Home for Residential Treatment
- Navigating Mental Health Treatment While in School
- Tips for Explaining Your Absence to Friends and Family
- Innovative Treatments in Mental Healthcare
- Mental Health Assessment and Diagnosis for Teens
- Contact Us