Mental Health Referrals From Hospitals: Post-Hospitalization Treatment for Teens

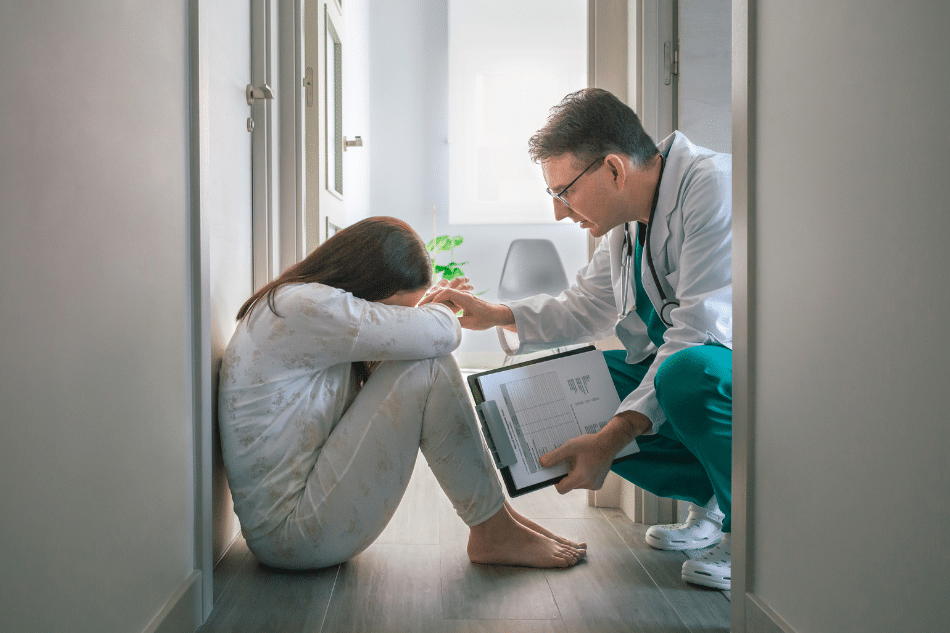
In the United States, around 15% of children’s hospital admissions are linked to psychiatric reasons.¹ When a teen is hospitalized for reasons such as this, it can be the start of a long journey of recovery.
What’s more, many families find out for the first time that their teen is struggling with mental health issues when they arrive at the emergency room. This can make it difficult to know what to do after the immediate danger has passed.
This is where mental health referrals from hospitals can make a difference, as they can open up the lines of communication and treatment after admission. These referrals connect families to post-hospitalization care, guiding teens toward stability, safety, and healing.
If you’re concerned about a teen’s continued care after mental health referrals from hospitals, a mental health professional can provide support and guidance. This page can also help, as it explores:
- How hospitals refer teens to treatment centers
- The importance of continuity of care when a teen is discharged from hospital
- The process of emergency psychiatric referrals for teens
- Types of post-hospitalization treatment for teens
- How Mission Prep can help with teen mental health stabilization programs
How Hospitals Refer Adolescents to Treatment Centers
Hospital systems take referrals seriously because discharge after mental health crises can be a vulnerable moment for teens. Therefore, once a child is medically stable, staff typically start to consider the next step, which could be:
- Outpatient therapy
- Residential care
- Inpatient mental health programs after crisis
This decision about what’s appropriate usually involves a team that includes psychiatrists, social workers, and case managers, and the process typically looks similar to the following:
- Assessment: Clinicians evaluate symptoms, risks, and history. If a suicide attempt occurred or if trauma is involved, a more structured program may be recommended. Additionally, if a teen is involuntarily admitted, inpatient care may be seen as the best route.²
- Collaboration: Hospitals often maintain open and communicative partnerships with mental health centers. These collaborations typically make referrals smoother and reduce delays in access to treatment.
- Parent Involvement: In the U.S., parents or guardians often have to consent to most post-crisis care for minors. Therefore, they are typically part of every referral discussion, unless the teen is over 18.
- Continuity of care: Families are provided with names of local therapists, adolescent post-crisis residential programs, or outpatient centers specializing in teen recovery.
In some cases, hospitals refer adolescents to treatment centers directly, securing the placement before discharge. In others, they provide emergency psychiatric referrals for teens, ensuring families have immediate contacts for specialized care. Either way, the goal is to prevent a relapse into crisis once the teen leaves the hospital doors.
The Importance of Continuity of Care Post Hospital Discharge for Teens
Research released in 2020 showed that a worrying percentage of adolescents had contemplated suicide. Plus, the same study showed that, between 2009 and 2015, mental health-related emergency room visits in pediatric patients increased by 56.4%.³ Therefore, it’s clear that continuity of care after hospitalization is essential for ongoing recovery.
In fact, receiving mental health care within 7 to 30 days of hospital release is associated with better outcomes. These include improved medication adherence, reduced suicide risk, and increased possibility of the patient continuing with long-term treatment.³
This information highlights how discharge from hospital is not the finish line. It’s the transition point. Continuity of care post hospital discharge is one of the most important predictors of whether a teen regains stability or returns to crisis.⁴ Gaps in care can lead to repeated hospitalizations, worsening symptoms, or unsafe behaviors.
However, continuity of care often looks different depending on the specific case. For instance, some teens step down into teen mental health stabilization programs, where daily therapy and medication management continue in a less intensive setting. Yet others may enter adolescent post-crisis residential programs, which combine therapy, academics, and family work. For lower-risk teens, outpatient counseling paired with medication follow-up may be enough.
Regardless of the setting, the aim is consistency. Post-hospitalization treatment for teens provides structure while the nervous system and emotional patterns recalibrate. Without this opportunity, the progress made in a hospital, such as medical stabilization before psychiatric treatment, can quickly unravel.
For families, continuity can also bring peace of mind. Knowing that support is in place after discharge may help parents feel bolstered and more secure during their child’s recovery.
The Process of Emergency Psychiatric Referrals for Teens
Emergency psychiatric referrals for teens often happen in frightening circumstances tied to a mental health condition. In these cases, ER physicians typically aim to stabilize the teen medically and immediately call in psychiatric staff for evaluation.
The following are some of the most common circumstances that trigger referrals from hospitals:
- Suicide attempts or suicidal ideation
- Acute panic attacks with physical collapse
- Psychotic breaks or hallucinations
- Severe trauma exposure, such as domestic violence or abuse
- Aggression or violence connected to an underlying psychiatric illness
In the United States, parental or guardian permission is typically required for minors under 18 to be admitted into ongoing treatment. However, in true emergencies, physicians can order inpatient psychiatric care after an ER visit without delay to ensure safety, while legal consent is being coordinated with guardians.
This process highlights the lifesaving role of mental health referrals from hospitals. Instead of sending a family home with uncertainty, these referrals provide clear direction about required care, whether this means a 72-hour psychiatric hold, longer inpatient care, or step-down outpatient support.
Types of Post-Hospitalization Treatment for Teens
Treatment after a hospital stay is not a one-size-fits-all approach. The referral depends on the severity of the crisis, family circumstances, and the teen’s ongoing needs.
Further, each program is designed to take the needs of the teen’s developing brain into account, offering different levels of structure, intensity, and family involvement. In other words, hospitals aim to match the right setting with the child’s unique developmental needs and psychiatric profile. When treatment is tailored in this way, there’s a reduced risk of relapse or repeated hospitalization.
The following are some of the most common types of post-hospitalization treatment for teens:
DBT for Teens Discharged From Hospitals
Dialectical behavior therapy (DBT) is an effective treatment for teens struggling with self-harm, suicidality, or extreme mood swings.⁵ Many hospitals recommend DBT for teens discharged from hospitals because it teaches:
- Practical coping skills
- Emotional regulation
- Resilience when distressed
- Healthier communication
By targeting these aspects, DBT often reduces the risk of relapse and helps stabilize family dynamics.
Sessions often combine individual therapy with group skill-building, giving teens the chance to practice strategies in real-world situations. Moreover, families are sometimes included in sessions to learn the same skills, which can help create more consistent support at home. Over time, DBT aims to help teens build resilience and a stronger sense of identity, which is critical after a psychiatric hospitalization.
Trauma Care After Hospital Psychiatric Admission
Teens hospitalized after trauma, such as domestic violence, abuse, or assault, often require specialized trauma care. This can include trauma-focused CBT (cognitive behavioral therapy), EMDR (Eye Movement Desensitization and Reprocessing), and group therapy.
Trauma care after hospital psychiatric admission provides a safe environment to process overwhelming experiences while building resilience. In fact, research shows that EMDR may be more effective for anxiety and PTSD (post-traumatic stress disorder) than CBT. However, both EMDR and CBT have been shown to be equally effective for treating depression.⁶
Therapists take care to design trauma programs in a way that’s well-paced, which can help avoid retraumatization and build coping skills. Peer trauma groups can also promote healing because they allow a teen to realize they’re not alone and that others have the same or similar struggles. Therefore, when post-hospital treatment includes trauma care, it can break negativity cycles, such as fear and avoidance, that often keep symptoms alive.
Suicide Attempt Recovery Treatment
For teens who were hospitalized after a suicide attempt, steps toward recovery tend to be both emotional and medical. For example, suicide attempt recovery treatment often includes:
- Individual therapy
- Psychiatric follow-up
- Family counseling
- Safety planning
These programs focus on teaching teens how to recognize warning signs and build stronger internal coping strategies.
Recovery also involves rebuilding hope and meaning, which requires more than symptom management. For instance, many programs emphasize creating “life worth living” plans, which include a teen’s goals, hobbies, and connections beyond crisis survival. Further, structured follow-up can reduce the risk of another attempt, which tends to be highest in the weeks immediately after hospitalization.
Inpatient and Residential Programs After Referrals From Hospitals
Some adolescents need more structure than outpatient settings can provide. Inpatient mental health programs after crises offer round-the-clock psychiatric monitoring and therapy. Additionally, longer-term residential treatment for abused teens or post-crisis youth weaves together therapy, school, and daily living skills. These programs can help teens regain a sense of safety while practicing independence.
Residential environments may also reduce environmental triggers by removing the teen from stressful or unsafe home situations. Plus, academic support ensures that treatment does not interrupt long-term goals like graduating from high school. Most importantly, these programs allow enough time for healing to happen, rather than expecting quick fixes.
Family Counseling After Teen Hospitalization
A teen’s healing process cannot happen alone. In most cases, family members are fearful or feel guilty and confused after a crisis. Family counseling after teen hospitalization helps parents and siblings understand what happened. It also helps the family unit rebuild trust and supportive communication skills after mental health crises.
For example, counseling can help parents respond to difficult behaviors without escalating conflict, which is essential in recovery. Siblings may also benefit from being included, as they often feel left out or confused by the hospitalization. Ultimately, family involvement creates a more stable home environment, which is one of the strongest predictors of long-term success. In fact, research shows that when family therapy is involved, treatment outcomes for teens are often better.⁷

Reach Out to Mission Prep for Advice on Teen Mental Health Stabilization Programs
If your teen has been discharged from a hospital after a psychiatric crisis, you may be feeling frightened and confused, and might need help figuring out the next steps. At Mission Prep, we specialize in guiding families through teen mental health stabilization programs and connecting them with the right level of care. From mental health referrals from hospitals to longer-term residential treatment, our team helps ensure that continuity of care is never broken.
Crisis may have brought your family to the hospital doors, but healing begins with the right follow-up care. Contact our team for further advice and guidance to get your teen the help they need.
References
- Joyce, V. W., King, C. D., Nash, C. C., Lebois, L. A. M., Ressler, K. J., & Buonopane, R. J. (2019). Predicting psychiatric rehospitalization in adolescents. Administration and Policy in Mental Health and Mental Health Services Research, 46(6), 807–820. https://pmc.ncbi.nlm.nih.gov/articles/PMC6886255/
- Rice, J. L., Tan, T. X., & Li, Y. (2021). In their voices: Experiences of adolescents during involuntary psychiatric hospitalization. Children and Youth Services Review, 126, 106045. https://www.sciencedirect.com/science/article/abs/pii/S0190740921001249
- Hugunin, J., Davis, M., Larkin, C., Baek, J., Skehan, B., & Lapane, K. L. (2023). Established outpatient care and follow-up after acute psychiatric service use among youths and young adults. Psychiatric Services, 74(1), 2–9. https://pmc.ncbi.nlm.nih.gov/articles/PMC9812848/
- Wong, B. H.-C., Chu, P., Calaminus, P., Lavelle, C., Refaat, R., & Ougrin, D. (2024). Association between continuity of care and attendance of post-discharge follow-up after psychiatric emergency presentation. NPJ Mental Health Research, 3(1), 5. https://pmc.ncbi.nlm.nih.gov/articles/PMC10955912/
- Kothgassner, O. D., Goreis, A., Robinson, K., Huscsava, M. M., Schmahl, C., & Plener, P. L. (2021). Efficacy of dialectical behavior therapy for adolescent self-harm and suicidal ideation: A systematic review and meta-analysis. Psychological Medicine, 51(7), 1057–1067. https://pmc.ncbi.nlm.nih.gov/articles/PMC8188531/
- Khan, A. M., Dar, S., Ahmed, R., Bachu, R., Adnan, M., & Kotapati, V. P. (2018). Cognitive behavioral therapy versus eye movement desensitization and reprocessing in patients with post-traumatic stress disorder: Systematic review and meta-analysis of randomized clinical trials. Cureus, 10(9), e3250. https://pmc.ncbi.nlm.nih.gov/articles/PMC6217870/
- Berry, K. R., Gliske, K., Schmidt, C., Ballard, J., Killian, M., & Fenkel, C. (2023). The impact of family therapy participation on youths and young adult engagement and retention in a telehealth intensive outpatient program: Quality improvement analysis. JMIR Formative Research, 7, e45305. https://pmc.ncbi.nlm.nih.gov/articles/PMC10160927/













