Key Takeaways
- Obsessive-Compulsive Disorder (OCD) in children and teens manifests as persistent, unwanted thoughts (obsessions) and repetitive behaviors (compulsions) that cause significant anxiety and interfere with daily functioning.
- Common signs include excessive handwashing, checking behaviors, fears of contamination, and a need for symmetry or order.
- Common tools for assessing OCD in children and teens include the Children’s Yale-Brown Obsessive Compulsive Scale (CY-BOCS).
- Effective management strategies include Cognitive Behavioral Therapy (CBT) and medication, with parental support playing a crucial role.
- Mission Prep provides specialized mental health treatment for teens with OCD through comprehensive evaluations, personalized plans, and proven therapies, all in a safe, supportive setting built for long-term healing.
OCD Checklist for Children & Teens: How to Spot The Main Signs
Understanding OCD
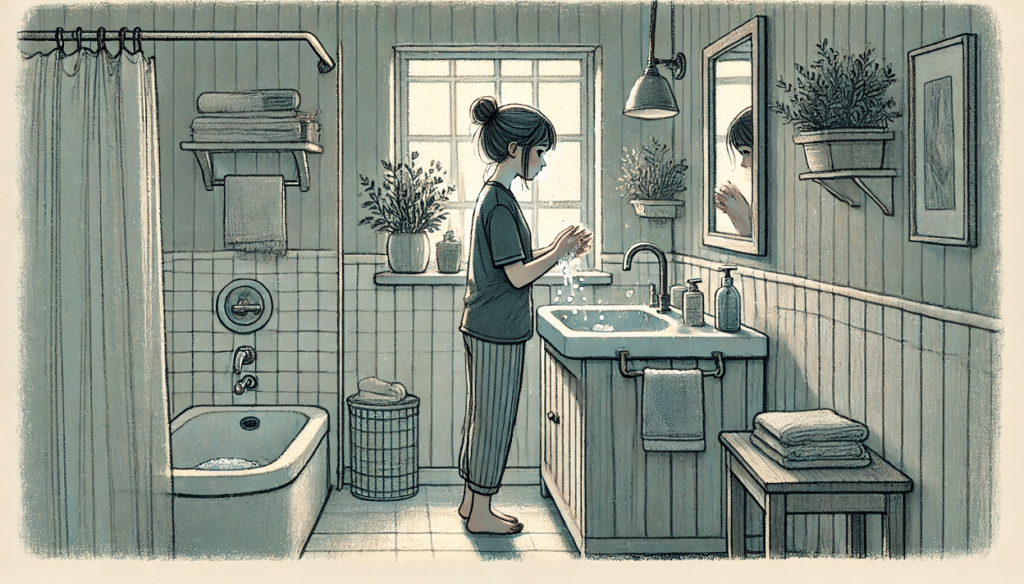
OCD is more than just liking things neat and tidy or having a few quirky habits. It’s a mental health disorder where obsessive thoughts lead to compulsive actions. For example, a teen might wash their hands excessively due to a fear of germs, even when their hands are already clean.
These obsessions and compulsions are not just temporary phases but can significantly impact daily functioning. That’s why recognizing these signs in children and teens is crucial.
Importance of Early Detection
Early detection of OCD allows for timely intervention, which can prevent the condition from worsening and help the child or teen lead a more fulfilling life. Besides that, early intervention can also reduce the risk of developing other mental health issues like anxiety or depression.
Mission Prep Healthcare specializes in mental health treatment for teens aged 12-17, offering residential and outpatient programs for anxiety, depression, trauma, and mood disorders. Our therapies include CBT, DBT, EMDR, and TMS, tailored to each adolescent’s needs.
With a structured, supportive environment, we integrate academic support and family involvement to promote lasting recovery. Our goal is to help teens build resilience and regain confidence in their future.
Common OCD Signs in Children & Teens
Obsessive Thoughts
Obsessive thoughts are intrusive, unwanted thoughts that repeatedly enter a person’s mind. For teens, these might include fears of contamination, harming others, or making mistakes.
Repetitive Behaviors
Repetitive behaviors, or compulsions, are actions performed to reduce the anxiety caused by obsessive thoughts. These can include:
- Frequent hand washing or cleaning rituals
- Checking things repeatedly, like locks or appliances
- Counting or repeating words silently
- Excessive fear of dirt or germs
- Need for symmetry or order
Anxiety & Distress
Anxiety and distress are often companions of OCD. The relentless cycle of obsessions and compulsions can be exhausting and overwhelming, leading to significant distress for the affected individual.
Causes & Triggers of OCD
Biological Factors
Research suggests that biological factors, such as differences in brain structure and function, might contribute to OCD. For instance, abnormalities in certain brain regions could influence the development of obsessive-compulsive behaviors.
Additionally, an imbalance of neurotransmitters, which are chemicals that transmit signals in the brain, has also been linked to OCD. Therefore, addressing these biological factors through appropriate treatment can be beneficial.
Genetic Influences
Studies have shown that OCD tends to run in families, suggesting a hereditary component. If a parent or sibling has OCD, there’s an increased likelihood that a child might develop it as well.
But genetics alone doesn’t determine the onset of OCD. They interact with other factors, such as environmental influences, to increase the risk. Therefore, understanding family history can be a valuable tool in assessing risk and managing OCD symptoms.
Environmental Contributors
Stressful life events, such as trauma or major changes, can trigger or worsen symptoms.

A teen who experiences bullying or a significant loss might see an increase in OCD symptoms.
Additionally, a family environment that is overly critical or lacks support can heighten anxiety, potentially triggering OCD behaviors. Creating a supportive and understanding environment is essential in managing OCD.
OCD Symptom Checklists for Children and Teens
Children’s Yale-Brown Obsessive Compulsive Scale (CY-BOCS)
The Children’s Yale-Brown Obsessive Compulsive Scale (CY-BOCS) is one of the most widely used tools for assessing OCD in children and teens. It measures the severity of obsessive and compulsive symptoms and helps track changes over time.
This scale consists of several items that evaluate the frequency and intensity of obsessions and compulsions. By using CY-BOCS, clinicians can better understand the impact of OCD on a child’s daily life and tailor treatment plans accordingly.
Obsessional Compulsive Inventory – Child Self Report (ChOCI-R-S)
The Obsessional Compulsive Inventory – Child Self Report (ChOCI-R-S) is a 32-item tool for identifying OCD symptoms in young individuals. Unlike CY-BOCS, this inventory is self-reported, allowing children and teens to express their experiences directly.
ChOCI-R-S covers a range of obsessive-compulsive symptoms and provides insights into the child’s perception of their condition. This self-reporting method empowers young individuals, giving them a voice in their diagnosis and treatment process.
Effective Management Strategies of OCD
Cognitive Behavioral Therapy (CBT)
Therapy is the first treatment option for OCD
Cognitive Behavioral Therapy (CBT) is a well-established treatment for OCD that involves identifying and challenging negative thought patterns and developing healthier coping mechanisms. CBT helps individuals understand the link between their thoughts, feelings, and behaviors.
Medication Options
In some cases, medication can be an effective part of an OCD treatment plan. Selective serotonin reuptake inhibitors (SSRIs) are commonly prescribed to help manage OCD symptoms by balancing neurotransmitters in the brain.
However, medication is not a one-size-fits-all solution. Work closely with a healthcare professional to determine the most suitable medication and dosage for each individual.
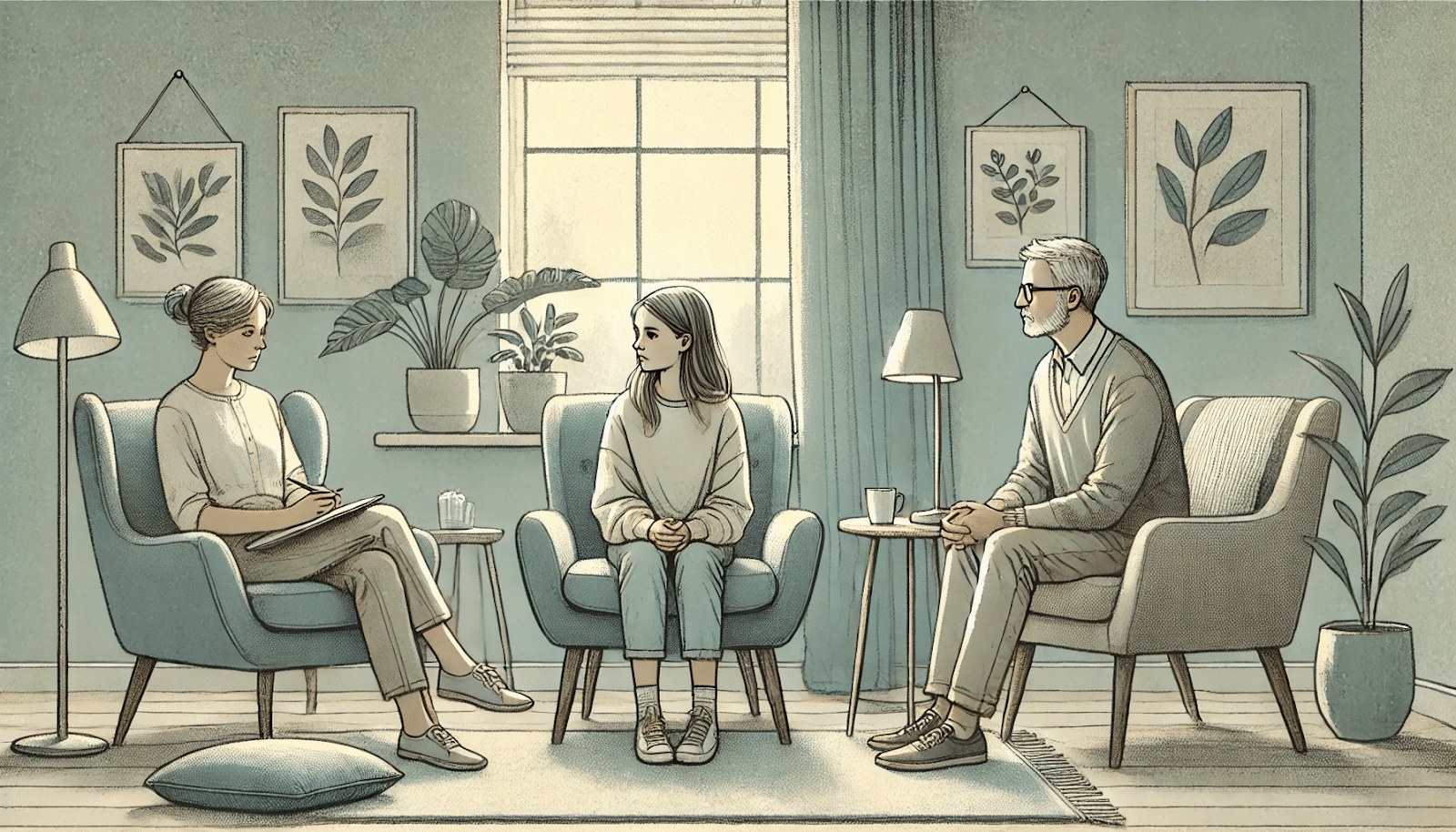
Parental Support and Intervention
Parents should provide a stable and understanding environment, helping their child manage the challenges of OCD. Encouraging open communication and actively participating in treatment can make a significant difference.
By working collaboratively with healthcare professionals, parents can help their child achieve better outcomes.
Seeking Professional Help
When to Consult a Specialist
If a child or teen is struggling to concentrate at school, socialize with friends, or complete everyday tasks, it’s time to seek help. Additionally, if there’s an increase in anxiety or distress, professional intervention is needed.
Additionally, early intervention can prevent symptoms from worsening and help the individual lead a more balanced life. Specialists, such as child psychologists or psychiatrists, can assess the severity of OCD and recommend appropriate treatment options.
Available Resources and Support
Various resources and support systems are available for families dealing with OCD. Mental health organizations, support groups, and online communities offer valuable information and a sense of community. These resources can provide insights into managing OCD and connecting with others who understand the challenges.
Mission Prep: Your Partner in OCD Treatment
Recognizing the signs of OCD in your child or teen is the first step toward healing. At Mission Prep, we understand that behind every checklist item is a young person experiencing real distress and a family seeking answers. Our approach to OCD treatment goes beyond symptom management—we address the whole person and the entire family system.
Our experienced team of mental health professionals conducts comprehensive evaluations to accurately diagnose OCD and develop personalized treatment plans tailored to each teen’s unique needs.
We use evidence-based therapies like CBT and Transcranial Magnetic Stimulation (TMS), which research consistently shows to be effective for OCD management. What sets us apart is our commitment to creating a safe, supportive environment where teens can heal.

Our modern facilities in California and Virginia provide the stability adolescents need while developing and practicing coping strategies.
If you’ve recognized OCD symptoms in your child, don’t wait to seek help. Contact Mission Prep today to learn how our specialized treatment approach can help your teen break free from the cycle of obsessions and compulsions and reclaim their life.
Frequently Asked Questions (FAQ)
How common is OCD in teens?
OCD affects approximately 1-2% of children and teens worldwide. It’s a relatively common mental health condition, and early diagnosis can lead to more effective management.
What triggers OCD episodes in children?
OCD episodes in children can be triggered by stress, changes in routine, or traumatic events. Additionally, certain environmental factors, such as family dynamics, can exacerbate symptoms.
Can OCD be cured in young individuals?
While there is no definitive cure for OCD, it can be effectively managed with the right treatment and support. Many young individuals experience significant improvement in symptoms through therapy, medication, and lifestyle changes.
How can parents support a child with OCD?
Parents can support a child with OCD by creating a stable and understanding environment. Encouraging open communication and actively participating in treatment can make a significant difference. Additionally, educating themselves about OCD enables parents to recognize triggers and support their child’s coping strategies effectively.
What treatment approaches does Mission Prep use for teens with OCD?
Mission Prep uses evidence-based approaches for treating OCD in teens, including CBT, TMS, medication when appropriate, family therapy, and comprehensive support services.
Our treatment plans are personalized to each teen’s specific symptoms and needs, with a focus on building sustainable coping skills and fostering family involvement throughout the recovery process.