Key Takeaways
- Trauma affects many adolescents and can manifest through behavioral, emotional, and physical symptoms that often go unrecognized.
- Key warning signs include social withdrawal, sleep disturbances, sudden mood changes, and declining academic performance.
- Physical manifestations such as unexplained aches, changes in appetite, and chronic fatigue may indicate underlying trauma.
- Adolescents may develop hypervigilance, avoidance behaviors, or flashbacks as part of post-traumatic stress responses.
- Mission Prep’s specialized team provides evidence-based trauma-informed treatments including EMDR, somatic experiences, and experiential therapies, all delivered through a strengths-based, resilience-focused approach customized to each teen’s unique needs.
Teen Trauma Warning Signs
Approximately 62% of all adolescents experience potentially traumatic events in their lifetime. These experiences range from witnessing violence to experiencing abuse, surviving accidents, or enduring ongoing neglect.
Trauma manifests differently in each adolescent, influenced by factors including personality, support systems, and the nature of the traumatic experience.
However, certain patterns emerge consistently across traumatized teens. Understanding these common indicators can help you, your parents, teachers, and other caregivers identify when you might be struggling with the aftermath of trauma rather than typical adolescent development.
Mission Prep Healthcare specializes in mental health treatment for teens aged 12-17, offering residential and outpatient programs for anxiety, depression, trauma, and mood disorders. Our therapies include CBT, DBT, EMDR, and TMS, tailored to each adolescent’s needs.
With a structured, supportive environment, we integrate academic support and family involvement to promote lasting recovery. Our goal is to help teens build resilience and regain confidence in their future.
Behavioral Red Flags
Withdrawal From Activities
One of the earliest and most common signs of trauma is a sudden disinterest in previously enjoyed activities. A teen who once enthusiastically participated in sports, music, or social clubs may begin making excuses to avoid these engagements.
This withdrawal often stems from emotional exhaustion, difficulty concentrating, or fear of triggering trauma reminders. In some cases, teens abandon activities specifically connected to their traumatic experience, while in others, they withdraw broadly as depression and anxiety take hold.
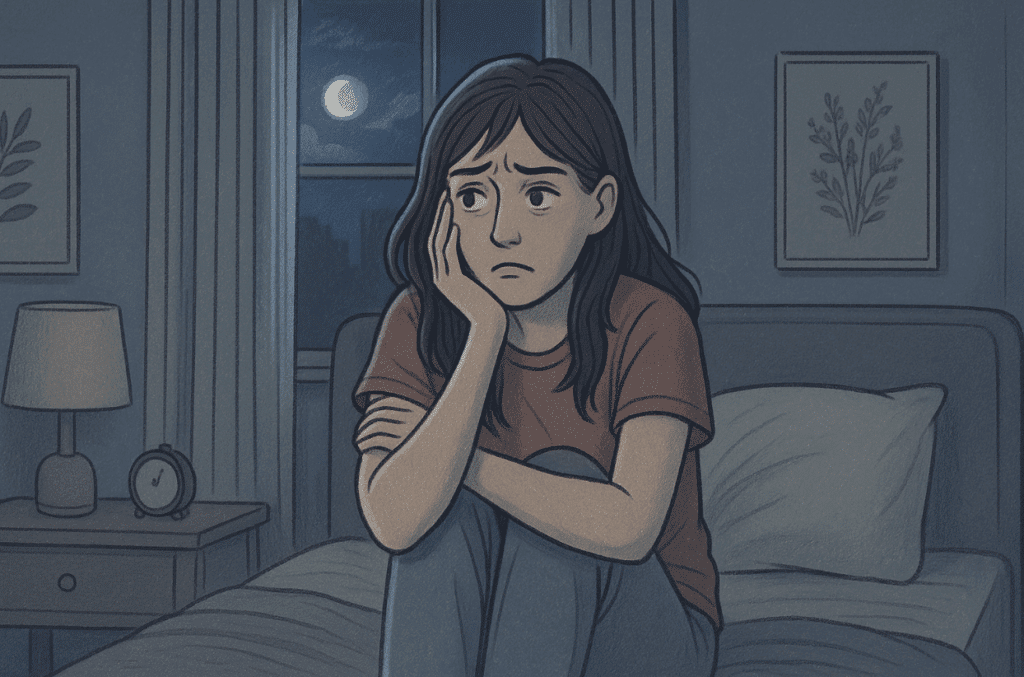
Sleep Disturbances
Trauma significantly disrupts sleep patterns in adolescents.
Some teens experience insomnia, lying awake ruminating about their experiences or staying up deliberately to avoid nightmares. Others may sleep excessively, using sleep as an escape mechanism from distressing thoughts and feelings.
You might experience perpetual exhaustion despite seemingly adequate sleep hours, suggesting poor sleep quality. Nightmares specifically related to the traumatic event are a particularly telling sign of post-traumatic stress.
Sudden Aggression
A previously calm teenager who begins displaying uncharacteristic anger, irritability, or even physical aggression may be processing trauma. This aggression often appears disproportionate to triggering situations, a minor inconvenience might provoke an intense outburst.
Behind this behavior typically lies heightened nervous system activation, making you quicker to perceive threats in your environment. Aggression can also serve as a protective mechanism, keeping others at a distance when you feel vulnerable.
Risk-Taking Behaviors
Traumatized teens frequently engage in dangerous behaviors that seem baffling to adults. Behaviors like reckless driving, sexual risk-taking, or self-harm might emerge suddenly.
These behaviors often represent attempts to numb overwhelming emotions or experience a sense of control. Some teens describe seeking “adrenaline rushes” to feel something beyond emotional numbness, while others use risk-taking as a form of self-punishment driven by trauma-related guilt or shame.
Academic Decline
A noticeable drop in academic performance frequently accompanies trauma in adolescents. Concentration difficulties, memory problems, and emotional distress make learning nearly impossible for some traumatized teens.
Assignments may go incomplete, or previously strong students might begin failing tests. Some teens avoid school altogether through truancy or frequent complaints of illness.
Emotional Indicators
Intense Mood Swings
Trauma can cause dramatic mood fluctuations that differ from typical teenage emotional variability.
A traumatized teen might appear calm one moment and intensely angry, sad, or anxious the next, often with minimal provocation. These mood swings reflect dysregulation in the brain’s emotional processing centers, making emotions feel overwhelming and difficult to control.
When mood changes persist for weeks or months and significantly impact daily functioning, they warrant professional attention.
Persistent Anxiety
Anxiety frequently becomes a constant companion for traumatized adolescents. This anxiety may manifest as excessive worry about everyday situations, frequent panic attacks, or persistent physical symptoms like stomach aches or headaches.
Many teens develop specific fears related to their traumatic experiences, a car accident survivor might refuse to ride in vehicles, while a bullying victim might develop social anxiety.
Emotional Numbness
Some traumatized teens appear emotionally flat or disconnected rather than overtly distressed. You might notice feeling “nothing” or “empty” when asked about your emotional state.
This numbness represents a protective psychological mechanism, when emotions become too overwhelming, the brain essentially shuts down emotional processing. While this provides temporary relief, prolonged emotional numbness prevents necessary processing of traumatic experiences.
Guilt or Shame
Intense guilt and shame frequently plague traumatized adolescents, even when they bear no responsibility for what happened. Teens might believe they could have prevented the traumatic event or blame themselves for not recovering more quickly.
These self-blaming thoughts can become persistent and intrusive, significantly damaging self-esteem.
Physical Symptoms
Unexplained Aches
Traumatized teens frequently report persistent physical pain without clear medical cause.
Headaches, stomachaches, muscle tension, and general malaise commonly accompany trauma responses. These symptoms stem from the body’s stress response system remaining chronically activated, causing inflammation and muscle tension.
The brain-body connection means emotional distress directly translates into physical sensations.
Fatigue
Persistent exhaustion plagues many traumatized adolescents, even with adequate sleep. This fatigue stems from the tremendous energy required to manage trauma responses and regulate emotions throughout the day. The body remains in a heightened state of alertness, depleting physical and mental energy reserves. Many teens describe feeling “worn out” or “drained” regardless of how much rest they get.
This exhaustion often impacts academic performance, athletic abilities, and social engagement. Teens might appear lazy or unmotivated when they’re actually experiencing trauma-related fatigue. Frequent requests to stay home from school or excessive napping may indicate this underlying trauma response rather than typical teenage behavior.
Changes in Appetite
Some teens lose appetite entirely, finding food unappetizing or feeling perpetual stomach distress that makes eating uncomfortable. Others develop emotional eating patterns, using food to self-soothe or numb difficult emotions.
These changes often lead to noticeable weight fluctuations that can create additional social and health concerns. Early intervention when appetite changes first appear can help prevent the development of more entrenched eating disorders.
Finding Healing With Mission Prep
Recognizing the signs of trauma in adolescence is the first critical step toward healing, but knowing where to turn for effective treatment makes all the difference. At Mission Prep, we understand that trauma affects teens across behavioral, emotional, and physical domains, requiring comprehensive, specialized care that addresses the whole person.

With our residential programs offering 24/7 support and structured environments, we provide the intensive care traumatized teens need while maintaining focus on their individual goals and sustainable recovery strategies.
Our trauma-informed approach goes beyond traditional therapy. We provide evidence-based treatments including EMDR and somatic experiences, integrated with experiential therapies like equine, art, and music therapy. Our entire team, from psychologists to our chef, receives trauma-informed training, ensuring every interaction supports healing and builds resilience.
What sets Mission Prep apart is our strengths-based, resilience-focused philosophy. We help teens understand that their trauma does not define their identity and that they possess the power to manage their experiences toward recovery. Our custom care plans address both single and compounded trauma, building practical skills and tools that support long-term healing.
Frequently Asked Questions
Can trauma symptoms appear years after the event?
Yes, delayed onset of trauma symptoms is quite common in adolescents. Some teens function relatively well immediately following traumatic events, only to develop symptoms months or even years later. This delay often occurs when teens initially use strong defense mechanisms like denial or dissociation to manage overwhelming experiences. Symptoms may emerge during periods of transition, stress, or when current situations trigger associations with previous trauma.
How can I tell if my teen’s behavior is trauma or normal adolescence?
The key differences lie in intensity, duration, context, and functional impact. Normal teenage moodiness tends to fluctuate, while trauma-related emotional changes appear more persistent and severe. Trauma-related behaviors typically don’t improve with standard parenting approaches and may worsen with traditional disciplinary measures. When behaviors significantly impair functioning across multiple life areas following known traumatic events, trauma should be considered as a potential underlying factor.
What should I avoid saying to a traumatized teen?
Avoid phrases that minimize their experience (“It could have been worse”), impose timelines on recovery (“You need to move on”), or suggest they should be grateful despite their trauma. Never demand forgiveness, force disclosure of details, or express disbelief about their experience. Instead, focus on validating feelings, emphasizing that trauma responses are normal reactions to abnormal situations, and expressing confidence in their capacity for healing with proper support.
Can trauma affect physical health in teenagers?
Trauma significantly impacts adolescent physical health through chronic stress responses that increase inflammation, disrupt hormones, and compromise immune function. Traumatized teens show higher rates of risky behaviors, and poor health habits. The chronic stress can contribute to autoimmune conditions, digestive problems, and chronic pain syndromes, with effects often persisting into adulthood if left untreated.
What types of therapy work best for adolescent trauma?
Evidence-based trauma treatments for adolescents include Trauma-Focused Cognitive Behavioral Therapy (TF-CBT), Eye Movement Desensitization and Reprocessing (EMDR), and Dialectical Behavior Therapy (DBT). At Mission Prep Healthcare we use these structured approaches to help teens process traumatic memories, develop coping skills, and address maladaptive thought patterns.