Key Takeaways
- Teen depression is a serious mental health condition, not just moodiness, and with timely support, most teens can recover and develop lifelong coping skills.
- While some cases improve naturally, early intervention significantly increases recovery chances and reduces risks like recurrence, substance use, and academic or social decline.
- Persistent, severe symptoms that impair daily functioning, such as school performance, relationships, or self-care, distinguish depression from typical adolescent mood swings.
- Recovery usually follows a gradual trajectory, with early improvements in weeks, substantial progress in months, and temporary setbacks are normal; consistent therapy, lifestyle changes, and family support improve outcomes.
- Mission Prep offers specialized, teen-focused, family-centered programs combining evidence-based therapy, academic support, and home-like environments to help adolescents overcome depression and build lasting resilience.
Teen Depression: What Parents and Teens Need to Know
Teen depression is a serious mental health condition affecting about 20% of adolescents by adulthood. It involves persistent sadness, hopelessness, and a loss of interest in activities, significantly impacting daily life.
Unlike normal sadness, clinical depression lasts at least two weeks and represents a noticeable change in functioning. Symptoms can include sleep and appetite changes, difficulty concentrating, and, in severe cases, thoughts of death or suicide.
The good news: teen depression is highly treatable. With proper support and intervention, most teens improve and develop coping skills that help them process challenges throughout life.
Mission Prep Healthcare specializes in mental health treatment for teens aged 12-17, offering residential and outpatient programs for anxiety, depression, trauma, and mood disorders. Our therapies include CBT, DBT, EMDR, and TMS, tailored to each adolescent’s needs.
With a structured, supportive environment, we integrate academic support and family involvement to promote lasting recovery. Our goal is to help teens build resilience and regain confidence in their future.
Does Teen Depression Actually Go Away on Its Own?
Parents often wonder if teen depression will fade with time. Research shows a nuanced but hopeful picture: while some cases improve naturally, most benefit significantly from professional support. Time alone rarely addresses the complex biological, psychological, and social factors behind depression, though teens’ natural resilience and supportive environments can aid recovery.
Natural Recovery Rates
Research shows that untreated depressive episodes often resolve naturally, with one study suggesting a median recovery time of 13 weeks for adolescents not receiving somatic therapy. However, recovery can vary widely depending on factors such as the severity of symptoms, social support, coping strategies, and coexisting conditions like anxiety or substance use.
Why Some Teens Bounce Back While Others Struggle
Long-term research has shown that the rate of recurrence in depressed youth is approximately 50% within two years and approximately 70% five years after diagnosis. Those with ongoing struggles often need more intensive or sustained support, but symptoms can still improve with effective treatment and coping strategies.
Factors Influencing Recovery
Several factors affect how depression progresses:
- Early intervention and active treatment engagement
- Symptom severity
- Quality of family support and social connections
- Co-occurring conditions like anxiety or substance use
- Genetic predisposition and family history
- Environmental stressors such as trauma or instability
These factors shape recovery paths but don’t dictate them. With proper care and support, many teens, even those with multiple risk factors, can achieve meaningful improvement.
Early intervention helps teens recover faster and develop lifelong coping skills.
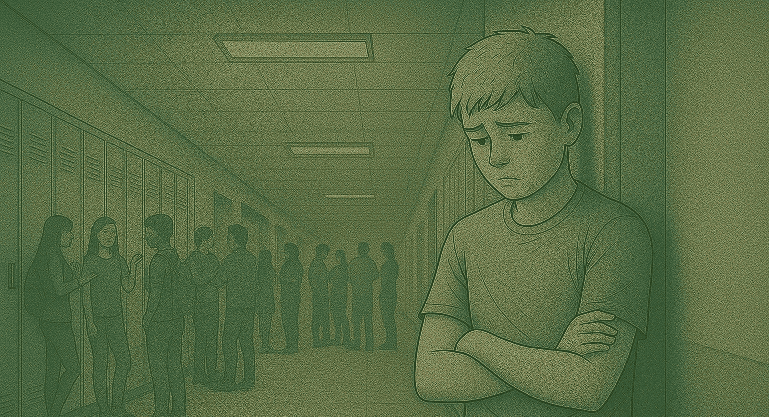
How to Tell Normal Teen Mood Swings from Clinical Depression
Adolescence naturally involves emotional ups and downs, making it challenging to distinguish typical moodiness from clinical depression. The key differences are persistence, severity, and the impact on daily life.
While normal teens may feel sad, irritable, or withdrawn occasionally, clinical depression lasts at least two weeks and represents a noticeable change from their usual behavior. It often affects multiple areas of life, including school performance, friendships, family relationships, and self-care.
Key Signs of Depression
Depressed teens may experience persistent feelings of emptiness, hopelessness, or irritability, lose interest in previously enjoyable activities, and withdraw from friends and family. They may also have noticeable changes in sleep, appetite, or energy, frequent physical complaints like headaches or stomachaches, and sometimes engage in risk-taking behaviors or self-harm. Thoughts of death or suicide, though less common, are serious warning signs.
Duration and Intensity
Temporary sadness from events like breakups or academic setbacks usually fades in days or weeks. Depression, by contrast, is ongoing, intense, and resistant to positive experiences. Teens may describe feeling “trapped,” “numb,” or like they are “wearing a mask,” struggling to manage daily life independently.
Impact on Daily Life
The most reliable indicator of depression is significant impairment in daily functioning. When emotional distress affects academics, social interactions, family life, or basic self-care, it’s likely more than typical teen moodiness, and professional support is essential.
Why Some Teen Depression Becomes Chronic
Some teens experience brief depressive episodes, while others develop more persistent depression. This difference stems from complex interactions between biological vulnerabilities, psychological factors, and environmental circumstances. Temporary depression often resolves as teens develop coping skills or as stressors improve, but chronic depression requires ongoing management.
Biological Risk Factors
Genetics plays a major role—teens with first-degree relatives who have experienced depression face a threefold higher risk. Neurobiological differences, including variations in serotonin, dopamine, and norepinephrine systems, affect mood regulation. Hormonal changes during adolescence, particularly in girls, can further increase vulnerability.
Environmental Triggers
Chronic stressors like family conflict, bullying, academic pressure, or social isolation worsen outcomes. Lack of supportive relationships and a problematic family environment can reinforce depression, while societal pressures and discrimination create additional burdens.
Early Trauma and Adverse Experiences
Adverse Childhood Experiences (ACEs) significantly increase depression risk. Trauma disrupts secure attachment and emotional regulation, creating patterns that heighten vulnerability. Timing matters: adversity during sensitive developmental periods can make depression more resistant to treatment.
The Spiral of Untreated Depression
Without intervention, depression can become self-perpetuating. Teens may withdraw socially, abandon activities, experience academic decline, and develop negative thought patterns that reinforce symptoms. Sleep disruption, poor nutrition, and reduced activity further erode resilience, turning episodic depression into a chronic condition.
Recovery Timeline: What to Expect
Families often wonder how long teen depression takes to improve and what patterns to expect. While recovery varies, understanding typical trajectories helps set realistic expectations and recognize progress.
Short-Term vs. Long-Term Recovery
Teens receiving appropriate treatment often show initial improvements within 4–6 weeks, such as subtle changes in energy, sleep, or engagement. More substantial gains typically appear within 3–4 months. For episodic depression without complicating factors, many teens achieve meaningful symptom reduction within 6–12 months, returning to generally positive functioning.
Complex cases, those with trauma history, co-occurring conditions, or severe symptoms, may follow a longer trajectory, with progress occurring gradually. Even then, significant improvement is common.
Signs of Improvement
Recovery usually follows a gradual upward trend rather than a straight line. Early recovery may include “good days and bad days,” with good days becoming more frequent over time. Functional improvements, better sleep, consistent school attendance, renewed social interest, and family engagement often signal meaningful progress. Returning to future-oriented thinking, such as making plans and setting goals, marks an important milestone.
Handling Setbacks and Relapses
Temporary setbacks are normal and don’t indicate failure. Stressful events or transitions can trigger symptom increases, but reinforcing coping skills helps maintain recovery. More significant relapses affect 30–40% of teens within two years, highlighting the importance of ongoing support. Returning to strategies that worked previously and early intervention during symptom recurrence can speed recovery and improve long-term outcomes.
Building Resilience to Prevent Future Episodes
Effective depression treatment alleviates current symptoms and helps teens develop resilience, reducing the risk of future episodes. Experiencing depression once increases the likelihood of recurrence, making these preventive skills especially important.
Coping Skills That Last
Treatment equips teens with psychological tools that serve them well beyond recovery. Cognitive restructuring helps challenge negative thought patterns, while emotional regulation teaches healthy ways to manage difficult feelings. Problem-solving skills encourage methodical approaches to challenges, and mindfulness fosters perspective and early recognition of warning signs. Communication skills, healthy boundary-setting, self-compassion, and stress management further strengthen coping capacity. Teens who master these skills often emerge with greater emotional intelligence than peers who haven’t faced similar challenges.
Creating a Depression-Resistant Environment
Environmental factors play a major role in relapse prevention. Maintaining regular sleep, consistent physical activity, and balanced nutrition provides biological support. Meaningful social connections serve as buffers against recurrence, emphasizing the importance of nurturing relationships alongside skill development.
Supportive families improve treatment outcomes through open communication and involvement.
When to Seek Professional Help
While teen depression often improves with treatment, parents may struggle to know when to seek help. Persistent changes in mood, behavior, or daily functioning lasting more than two weeks, especially across multiple areas of life, warrant professional evaluation.
Warning Signs Requiring Immediate Attention
Urgent evaluation is needed for any suicidal thoughts or talk, self-harming behaviors, dramatic personality changes, or signs of psychosis (hallucinations or severe paranoia). Significant functional decline, such as refusing school, isolating from peers, or neglecting basic self-care, also signals serious depression. Persistent or severe physical symptoms without a clear medical cause may indicate depression needing treatment.
Finding the Right Mental Health Provider
Treatment effectiveness depends on working with the right professional. A comprehensive evaluation by a mental health provider experienced in adolescent depression, such as a child and adolescent psychiatrist, psychologist, or licensed therapist, provides the foundation for an effective, tailored treatment plan.
Mission Prep: Supporting Adolescents Every Step of the Way
Mission Prep offers specialized mental health care exclusively for adolescents aged 12–17, combining clinical expertise with a family-centered approach. Our programs focus on helping teens process depression, anxiety, trauma, mood disorders, and social or academic challenges while developing lifelong coping skills.

Mission Prep empowers teens to have a “vote and voice” in their treatment journey.
Family-Centered Approach
Families are active partners in treatment, with teens encouraged to have a “vote and voice” in their care. Weekly family therapy, regular communication, and support resources ensure the entire family system is engaged in recovery.
Comprehensive Programs and Therapies
Mission Prep provides residential, outpatient, and virtual programs, blending evidence-based therapies like Cognitive Behavioral Therapy (CBT), Eye Movement Desensitization and Reprocessing (EMDR), and Transcranial Magnetic Stimulation (TMS) with individuals, groups, and families to address a range of adolescent mental health needs.
Academic Support and Home-Like Settings
Programs include integrated academic coordination, allowing teens to continue their education. Licensed, home-like environments feature semi-private rooms, shared meals, and peaceful surroundings, with a 3:1 staff ratio including master’s- and doctorate-level clinicians, plus onsite doctors and psychiatrists.
Sustainable Recovery and Locations
The focus is on long-term skills and resilience rather than short-term fixes. Mission Prep operates in California and Virginia, preparing teens to thrive well beyond treatment.
Frequently Asked Questions (FAQs)
Can teens develop depression from social media use?
Excessive or negative social media use, over three hours daily, nighttime activity, or comparison-focused browsing, can increase depression risk. Balanced use that fosters connection and positive engagement may support mental health instead of worsening symptoms.
Is teen depression more common now than in previous generations?
Teen depression rates have risen significantly, especially since 2012, affecting girls disproportionately. Contributing factors include increased awareness, diagnostic improvements, academic and social pressures, digital media, family changes, and reduced stigma around reporting mental health concerns.
Will my teen need to take antidepressants for life if they start them?
Most teens do not need lifelong antidepressants. Typically, medication continues 6–12 months after recovery. Duration depends on depression severity, recurrence risk, family history, and coping skills, with many teens eventually tapering under medical supervision.
How can I approach my teen if I think they’re depressed but they won’t talk about it?
Use patient, non-confrontational communication during relaxed, low-pressure moments. Share observations, listen without judgment, validate feelings, and offer support. If resistant, suggest indirect resources like articles, online services, or appointments, while consistently expressing care.
Can teen depression come back in adulthood?
Depression in adolescence can increase the risk of recurrence in adulthood, with roughly 40–70% experiencing another episode by age 30. Teens who receive early, structured support, such as programs at Mission Prep, often develop coping strategies that help them manage future episodes more effectively, reducing long-term impact.