Key Takeaways
- Major depressive disorder in teens goes beyond typical mood swings, involving persistent sadness, loss of interest, and changes in daily functioning that last for weeks or months.
- Recognizing symptoms early is crucial, as teen depression manifests through emotional withdrawal, behavioral changes, physical complaints, and declining academic or social performance.
- Therapy-based treatments like Cognitive-Behavioral Therapy (CBT), Dialectical Behavior Therapy (DBT), and Interpersonal Therapy (IPT) effectively address teen depression by building coping skills and reshaping thought patterns.
- Family involvement and comprehensive treatment that addresses underlying causes create the strongest foundation for lasting recovery from MDD.
- Mission Prep’s integrated residential, outpatient, and telehealth programs combine evidence-based therapies with family support to provide personalized treatment for teens ages 12–17 struggling with major depressive disorder.
Understanding Major Depressive Disorder in Teenagers
Major depressive disorder (MDD) in teenagers is a serious mental health condition that affects how adolescents think, feel, and function in their daily lives. Unlike occasional sadness or mood fluctuations that are part of normal adolescent development, MDD involves persistent symptoms that interfere with school, relationships, and overall well-being.
The teenage years naturally bring emotional ups and downs as adolescents navigate identity development, social pressures, and biological changes. However, MDD represents something more significant. It’s a clinical condition characterized by prolonged periods of depression that don’t simply resolve on their own.
Understanding the difference between normal teenage moodiness and clinical depression helps families recognize when professional support is needed. While all teens experience difficult emotions, MDD creates patterns of symptoms that persist over time and significantly impact multiple areas of life. Early recognition and appropriate treatment make a meaningful difference in helping teens recover and build resilience.
Mission Prep Healthcare specializes in mental health treatment for teens aged 12-17, offering residential and outpatient programs for anxiety, depression, trauma, and mood disorders. Our therapies include CBT, DBT, EMDR, and TMS, tailored to each adolescent’s needs.
With a structured, supportive environment, we integrate academic support and family involvement to promote lasting recovery. Our goal is to help teens build resilience and regain confidence in their future.
Recognizing the Symptoms of Teen Depression
Major depressive disorder manifests through various symptoms that affect emotions, behavior, physical health, and social functioning. Because teens may express depression differently than adults, parents benefit from understanding the full range of warning signs.
Emotional symptoms often include persistent sadness, feelings of emptiness, or disproportionate irritability. Teens with MDD may express feelings of worthlessness, excessive guilt about minor mistakes, or hopelessness about the future. They might cry frequently or appear emotionally numb.
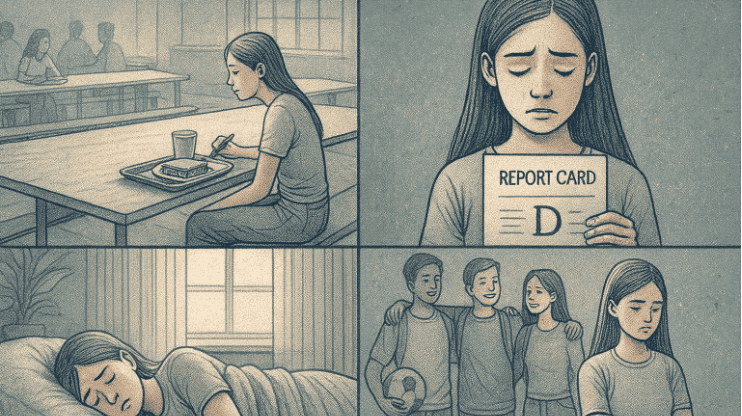
Behavioral changes frequently signal depression in adolescents, including withdrawing from friends and family, losing interest in once-enjoyed activities, and isolating themselves. Academic performance may decline as concentration difficulties make schoolwork challenging. Some teens become more aggressive or engage in risky behaviors.
Physical symptoms can be prominent in teen depression, including sleep pattern changes, persistent fatigue despite adequate rest, and unexplained physical complaints like headaches or stomachaches. Changes in appetite and weight often accompany depression.
Social withdrawal represents another key indicator. Teens with MDD may stop participating in extracurricular activities, avoid social gatherings, or struggle to maintain friendships, leading to increased isolation that reinforces depressive symptoms.
Understanding the diverse symptoms of teen depression helps families recognize when their adolescent needs professional support and treatment.
What Causes MDD in Adolescents
Major depressive disorder in teens typically develops from a combination of biological, psychological, environmental, and social factors. Understanding these contributing elements helps families recognize that depression is a complex condition rather than a character flaw.
Biological factors play a significant role in adolescent depression. Brain chemistry differences, particularly involving neurotransmitters that regulate mood, can make some teens more vulnerable. Family history of depression also increases risk, suggesting genetic components that influence mental health susceptibility. Hormonal changes during puberty affect mood regulation, and the teenage brain is still developing areas responsible for emotional regulation.
Environmental stressors often trigger or worsen depression. Academic pressure, social conflicts, bullying, or peer relationship difficulties create chronic stress that overwhelms coping abilities. Major life transitions like moving to a new school, parental divorce, or loss of important relationships can precipitate depressive episodes.
Trauma and adverse experiences significantly impact mental health. Teens who have experienced abuse, neglect, or witnessed violence carry additional risk factors. Even less obvious stressors, like chronic family conflict or feeling emotionally invalidated, contribute to depressive symptoms.
Social media and technology present unique modern challenges. Constant social comparison, cyberbullying, and pressure to maintain certain images online can fuel feelings of inadequacy and isolation. Perfectionism and high self-expectations also contribute, as adolescents who place intense pressure on themselves may develop depression when perceiving themselves as falling short.
Therapy-Based Treatment Options
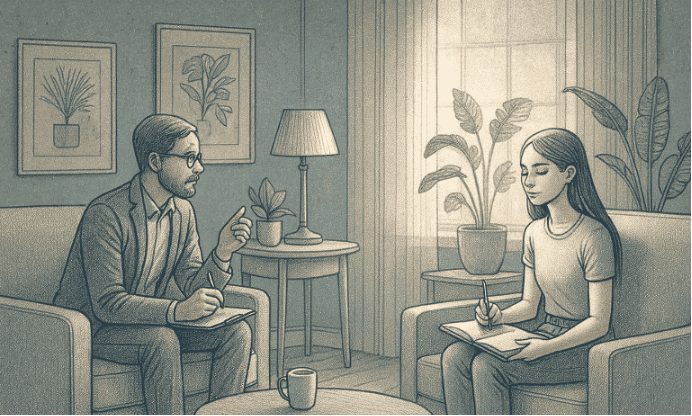
Effective treatment for teen depression centers on evidence-based therapeutic approaches that help adolescents develop coping skills, reshape thought patterns, and build emotional resilience. These treatments address both current symptoms and underlying contributing factors.
Cognitive-Behavioral Therapy (CBT) is one of the most effective approaches for treating teen MDD. CBT helps adolescents identify negative thought patterns that fuel depression and learn to challenge and replace them with more balanced perspectives. Teens learn to recognize connections between thoughts, feelings, and behaviors, developing practical skills for managing difficult emotions. The structured approach provides concrete tools that teens can use independently, creating lasting change.
Dialectical Behavior Therapy (DBT) offers particularly valuable tools for teens who experience intense emotions or struggle with emotional regulation. DBT teaches four core skill sets: mindfulness for staying present and aware, distress tolerance for managing crisis situations, emotion regulation for understanding and modifying intense feelings, and interpersonal effectiveness for navigating relationships. These skills help teens build healthier ways of coping with emotional pain.
Interpersonal Therapy (IPT) focuses on improving relationship patterns and communication skills that affect mood. This approach recognizes that teen depression often involves interpersonal struggles like conflicts with parents or peers, grief and loss, life transitions, or social isolation. IPT helps adolescents develop more effective ways of relating to others and building supportive connections.
Group therapy provides additional benefits by allowing teens to connect with peers facing similar challenges. Sharing experiences in a safe environment reduces isolation and helps teens realize they’re not alone. Group settings also provide opportunities to practice social skills and receive peer support.
Evidence-based therapies give teens practical tools and skills for managing depression, building emotional resilience, and creating lasting positive change.
The Role of Family Therapy and Support
Family involvement significantly strengthens treatment outcomes for teens with major depressive disorder. Depression affects the entire family system, and recovery happens more effectively when families work together to create supportive environments and healthier communication patterns.
Family therapy helps address dynamics that may contribute to or maintain depressive symptoms. Sometimes, family conflict, communication difficulties, or unresolved tensions create stress that affects the teen’s mental health. Family therapy provides a space to improve understanding, develop more effective communication strategies, and strengthen bonds.
Parents benefit from education about teen depression, learning to distinguish between symptoms of the disorder and typical adolescent behavior. Understanding depression as a medical condition helps families respond with compassion and appropriate support rather than frustration or criticism. Parents also learn how to support recovery without becoming overly involved or inadvertently reinforcing depressive behaviors.
Creating a home environment that supports recovery involves establishing consistent routines, maintaining open communication, reducing criticism and conflict, and celebrating progress. Families learn to recognize warning signs of worsening symptoms and develop plans for responding effectively.
Why Mission Prep’s Comprehensive Approach Works

Mission Prep treats teen depression with a full continuum of care: residential, outpatient, and telehealth, combining CBT, DBT, IPT, and family work in a peaceful environment.
When teenage depression requires professional treatment, Mission Prep Healthcare offers specialized programs that integrate multiple therapeutic approaches for effective, lasting recovery.
Our programs serve adolescents ages 12 to 17 through residential, outpatient, and telehealth services designed specifically for teen mental health needs. We understand that major depressive disorder requires comprehensive treatment addressing not just symptoms but underlying causes and contributing factors.
Our therapeutic approach combines evidence-based treatments like Cognitive-Behavioral Therapy, Dialectical Behavior Therapy, and Interpersonal Therapy with family involvement and skill-building programs. This integrated model ensures teens develop practical tools for managing depression while families learn to provide effective support.
We emphasize creating lasting change through skill development rather than temporary symptom relief. Teens learn emotion regulation techniques, healthy coping strategies, and resilience-building practices they can use throughout their lives.
Our family-focused approach recognizes that successful treatment involves the entire family system. We provide education, support, and guidance to help families create home environments that support sustained mental health.
Frequently Asked Questions (FAQ)
How long does treatment for teen MDD typically take?
Treatment duration varies based on symptom severity and individual progress, but most teens begin experiencing improvement within several weeks of starting therapy. Comprehensive treatment often continues for several months to ensure lasting change and prevent relapse. Many teens benefit from ongoing support even after initial symptoms improve.
Can therapy alone effectively treat major depressive disorder in teens?
Therapy-based treatments like Cognitive-Behavioral Therapy and Dialectical Behavior Therapy are highly effective for treating teen depression, helping adolescents develop coping skills and address underlying factors contributing to their symptoms. The most effective approach depends on each teen’s specific situation and needs.
How can I support my teen with depression at home?
Supporting a teen with depression involves maintaining open, non-judgmental communication, educating yourself about the condition, encouraging treatment participation, helping maintain healthy routines, and taking care of your own mental health. Avoid minimizing their feelings or offering quick fixes, and instead provide a consistent presence and understanding.
What programs does Mission Prep offer for teens with major depressive disorder?
Mission Prep provides residential, outpatient, and telehealth programs specifically designed for adolescents ages 12–17 experiencing major depressive disorder and related mental health challenges. Our comprehensive approach integrates evidence-based therapies, family support, and skill-building programs that address both depression symptoms and contributing factors for lasting recovery.