Key Takeaways
- Teen girls are particularly vulnerable to PTSD due to higher exposure to trauma, biological differences in stress response, and hormonal fluctuations that intensify traumatic memories.
- PTSD symptoms in teens often show as extreme mood swings, social withdrawal, sleep problems, physical complaints, or changes in academic performance rather than explicit discussion of trauma.
- Early, sensitive intervention is crucial—approach teens with observation, empathy, and patience, focusing on feelings rather than behaviors, and normalize seeking professional help.
- Effective treatment combines evidence-based therapies like TF-CBT and EMDR, complemented by supportive activities and, if needed, medication, helping teens rebuild coping skills and emotional regulation.
- Mission Prep offers teen-only programs with evidence-based therapy, family involvement, academic support, and safe, structured environments to help adolescents recover and build resilience.
PTSD in Teen Girls: What Parents Need to Know
PTSD develops when trauma overwhelms a teen’s ability to cope. For teenage girls, this can stem from experiences like assault, bullying, witnessing violence, or serious accidents. These events can alter how the adolescent brain processes and regulates emotions.
Unlike adults, teens often lack the vocabulary to recognize their symptoms. Many internalize their trauma, assuming their reactions are part of who they are, which can lead to self-blame and delay treatment. Parents should note that symptoms may appear as behavioral changes, physical complaints, or academic struggles rather than direct talk of flashbacks. With proper care, however, teen girls can recover and demonstrate remarkable resilience.
Mission Prep Healthcare specializes in mental health treatment for teens aged 12-17, offering residential and outpatient programs for anxiety, depression, trauma, and mood disorders. Our therapies include CBT, DBT, EMDR, and TMS, tailored to each adolescent’s needs.
With a structured, supportive environment, we integrate academic support and family involvement to promote lasting recovery. Our goal is to help teens build resilience and regain confidence in their future.
Why Teen Girls Are More Vulnerable to PTSD
Teen girls face a unique set of risk factors that contribute to their higher rates of PTSD. Research shows they are more likely to experience sexual violence and relationship abuse traumas, with especially high risks for PTSD. They are also more often exposed to ongoing or repeated trauma, which complicates recovery. Beyond exposure, biological differences matter. The female brain links fear and memory more strongly, making traumatic memories feel vivid and intrusive. Hormonal fluctuations, particularly during adolescence, can further intensify symptoms.
Higher Risk Factors
Teen girls face environmental and social risks that heighten vulnerability to PTSD. Society encourages a stronger relationship focus, which can make interpersonal trauma more damaging. Many girls also use ruminative coping, dwelling on distress, which reinforces trauma instead of processing it.
Biological Differences in Stress Response
Girls show different stress patterns than boys. While boys often display “fight-or-flight,” girls tend toward “tend-and-befriend,” seeking connection under stress. Trauma that breaks trust disrupts this natural response, creating deeper emotional pain.
Social Pressures and Trauma Processing
Cultural expectations around emotions complicate recovery. Girls are pressured to be expressive but not “too emotional,” leading to suppression or dismissal of real distress. These scenarios often delay recognition and treatment of PTSD in teen girls.
Recovery isn’t linear, but with compassion and care, teens can thrive beyond trauma.
8 Signs of PTSD in Teen Girls
Understanding the signs of PTSD in teen girls can be challenging, as many symptoms overlap with typical adolescent behavior. Recognizing the differences is key to early support and intervention.
1. Sudden Changes in Mood and Irritability
PTSD often causes extreme, unpredictable mood swings that go beyond normal teen ups and downs. Anger may escalate into explosive outbursts or aggression triggered by trauma reminders. These episodes can seem irrational but reflect the nervous system’s fight-or-flight response. Teens may also show prolonged irritability, snapping over minor stressors, or withdrawing emotionally, leaving parents and friends confused or concerned.
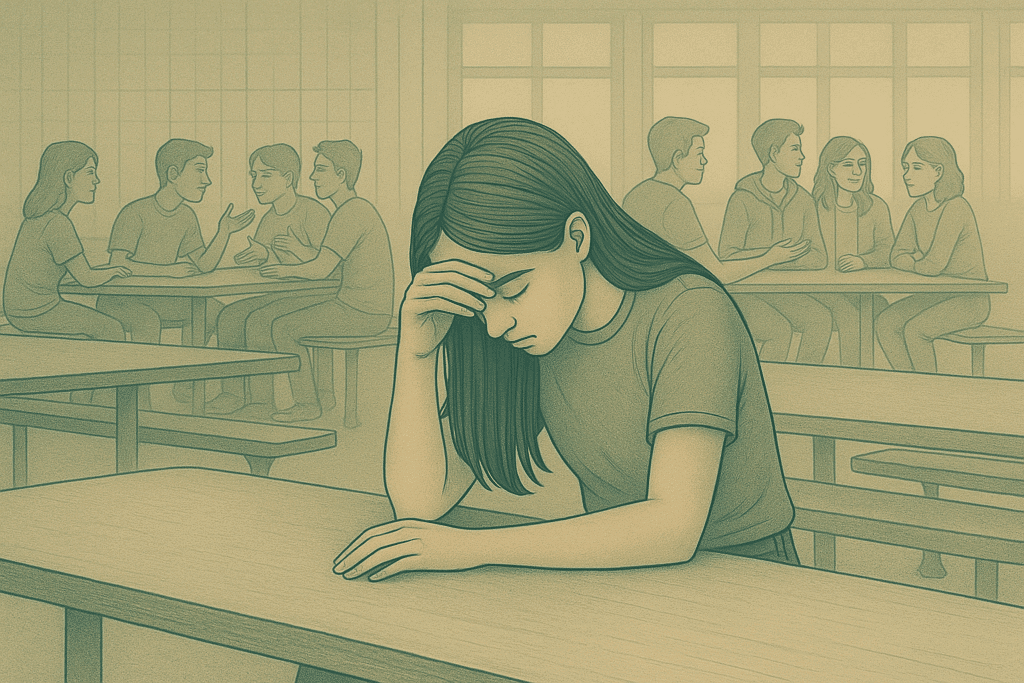
2. Withdrawal From Friends and Activities
Unlike typical shifting interests, PTSD withdrawal is more profound. Teens may isolate themselves from friends, avoid social events, and lose interest in hobbies they once loved. This disconnection stems from emotional numbness, avoidance of trauma reminders, or feeling unsafe in relationships. Parents may notice increased time alone, reluctance to attend family activities, or declining school participation, which can worsen feelings of isolation.
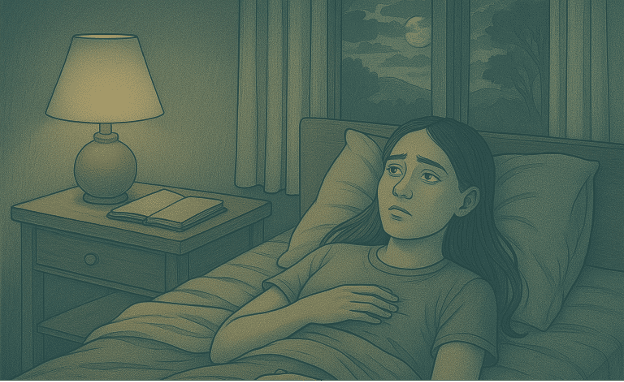
3. Sleep Problems and Nightmares
Disturbed sleep is a hallmark of PTSD. Teens may struggle to fall asleep, wake repeatedly, or fear going to bed due to vivid nightmares and night terrors. Nightmares often replay aspects of trauma, leaving the teen fearful, restless, and exhausted. Over time, insomnia and sleep avoidance reduce emotional regulation, intensifying irritability, anxiety, and difficulty concentrating during the day.
4. Physical Complaints Without Medical Cause
PTSD often manifests through unexplained physical symptoms like headaches, stomachaches, fatigue, or muscle tension. These complaints are real, caused by a dysregulated stress response and constant activation of the body’s fight-or-flight system. Hormonal fluctuations during adolescence may amplify these symptoms, which can lead to missed school days or decreased participation in daily activities.
5. Flashbacks and Intrusive Memories
Flashbacks make trauma feel like it’s happening again, sometimes subtly, sometimes vividly. Teens may zone out, show distress without a clear cause, or experience racing hearts, sweating, or trembling. Triggers can be sensory, situational, or even online content. Partial flashbacks, where teens seem functional but are internally distressed, are common and can be confusing for both the teen and caregivers.
6. Academic Performance Changes
Trauma impacts focus, memory, and learning. Teens may appear distracted, forgetful, or inconsistent in schoolwork. This isn’t laziness, it’s the brain prioritizing survival over concentration. Hyperarousal and intrusive thoughts make multi-step tasks harder, while working memory struggles can make previously manageable assignments feel overwhelming. Parents and teachers may notice sudden drops in grades, incomplete homework, or difficulty following lessons.
7. Hypervigilance and Startle Responses
Many teens remain on constant alert, scanning for danger even in safe places. They may avoid crowds, insist on facing exits, or overreact to sudden noises. This heightened state of alertness consumes energy, causing fatigue, irritability, and sleep problems. Even ordinary sounds or movements can trigger exaggerated startle responses, leading to avoidance behaviors that reinforce anxiety and hyperarousal.
8. Self-Destructive Behaviors
To cope with overwhelming pain, some teens turn to risky behavior, substance use, or self-harm. These actions are attempts to manage distress, not attention-seeking. Teens may engage in reckless activities, experiment with drugs or alcohol, or injure themselves to relieve emotional pain or regain a sense of control. Early recognition, compassionate support, and trauma-focused therapy are essential to replace harmful coping strategies with healthier ones.
How to Approach a Teen You Suspect Has PTSD
Approaching a teen about possible PTSD requires sensitivity and careful timing. Choose a private, calm moment when neither of you is rushed, and remember your goal is to open communication and convey unconditional support—not to diagnose or solve problems immediately.
- Lead with observations, not accusations: “I’ve noticed you seem tired lately” instead of “Why are you always tired?”
- Normalize help-seeking: “Many teens find talking to someone helpful when they’re going through tough times.”
- Offer options, not mandates: “There are different ways to get support. Would you like to hear about some?”
- Respect her pace: “It’s okay if you’re not ready to talk now. I’m here whenever you are.”
- Focus on feelings: “How have you been feeling lately?” instead of “Why are you skipping school?”
Teens with PTSD often feel shame and may deny or minimize symptoms as a self-protective response. Avoid pressuring them, leave the door open by checking in periodically, and model healthy emotional communication.
Early intervention improves outcomes and prevents secondary problems like substance use or depression. If symptoms persist for more than a month, consider consulting a mental health professional, even if your teen isn’t ready to participate directly. Be honest about limits: “I’ll respect your privacy, but your safety comes first. If I’m worried you might be in danger, we’ll get help together.”
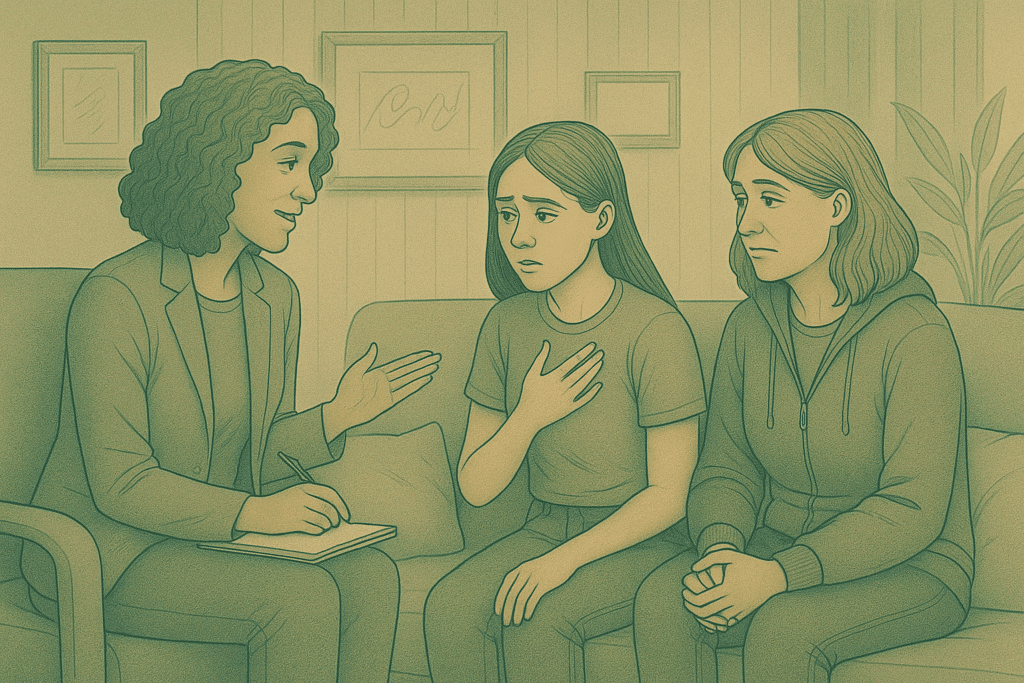
Family involvement reinforces recovery and provides teens with steady emotional anchors.
Creating a Safe Space for Communication
Consistency builds trust. Establish predictable moments for connection, shared activities, regular meals, or quiet time—without pressuring her to discuss difficult topics. When she chooses to share,she minimizes distractions and gives full attention.
Phrases That Help Rather Than Harm
- “I believe you.” Validates experiences and rebuilds trust.
- “This wasn’t your fault.” Counters self-blame and helps disrupt harmful thought patterns.
Setting Boundaries While Showing Support
Compassion works best with clear boundaries. Communicate expectations around safety, school, and family responsibilities, while remaining flexible during difficult periods. For example, maintain school attendance expectations but allow accommodations like reduced course load or breaks when overwhelmed. This balance fosters resilience while providing needed support.
Treatment Options That Really Work
Effective treatment for PTSD in teen girls usually combines several approaches specific to their symptoms, trauma history, and preferences. While therapy may feel intimidating, research shows professional treatment is far more effective than a “wait and see” approach. Adolescents often respond quickly due to the brain’s neuroplasticity, allowing new pathways for healing.
Evidence-Based Therapies for Teen PTSD
Trauma-Focused Cognitive Behavioral Therapy (TF-CBT) helps teens identify and challenge trauma-related thoughts, develop coping skills, and safely process memories. Its clear structure provides a sense of control over symptoms.
Eye Movement Desensitization and Reprocessing (EMDR) uses guided eye movements to help the brain reprocess traumatic memories, reducing their emotional intensity. This can be ideal for teens who struggle to verbalize their experiences or find talk therapy overwhelming.
When Medication Might Be Necessary
Medication is considered when symptoms severely impair daily functioning or therapy engagement. SSRIs have the strongest evidence for adolescent PTSD, especially for hyperarousal, intrusive thoughts, or comorbid depression. Medication works best alongside therapy, not as a standalone solution. Providers typically start with low doses, monitor closely for side effects, and adjust treatment as needed, helping restore emotional regulation without fundamentally changing personality.
Complementary Approaches That Support Recovery
Body-based interventions like yoga, dance, or martial arts help teens reconnect with their bodies, regulate physical stress responses, and build confidence.
Expressive arts therapies, including visual art, music, drama, and writing, allow teens to process trauma creatively when words feel insufficient, promoting healing while boosting self-efficacy.
Supporting Teens Through Recovery with Mission Prep
Healing from trauma and mental health challenges can be overwhelming, but Mission Prep Healthcare provides a safe, structured, and teen-focused environment for adolescents aged 12–17. Their programs are designed to help teens regain stability, build resilience, and face challenges like anxiety, depression, trauma, mood disorders, and technology dependence.

Balancing structure and support allows teens to face fears while feeling safe.
Why Mission Prep Stands Out:
- Teen-Only Programs: All services are tailored specifically for adolescents, ensuring therapy, social activities, and academic support are developmentally appropriate.
- Evidence-Based Therapies: Teens engage in CBT, DBT, EMDR, and TMS, which help process trauma, manage emotions, and develop coping skills.
- Integrated Academic Support: Treatment includes educational coordination, so learning continues uninterrupted, supporting both mental health and academic growth.
- Family-Centered Care: Families are actively involved through weekly therapy, structured communication, and transition planning, reinforcing healing at home.
- Safe, Home-Like Settings: Licensed group homes with semi-private rooms, shared meals, and a structured environment help teens feel secure and supported.
Mission Prep offers residential, outpatient, and virtual programs across California (Rancho Palos Verdes, Rolling Hills Estates) and Virginia (Waterford and surrounding areas), providing flexible care for teens at different stages of recovery.
Frequently Asked Questions (FAQs)
Can PTSD go away on its own in teenagers?
Full PTSD rarely resolves without treatment. While mild trauma responses may improve with time and support, persistent symptoms interfering with daily life require professional intervention. Untreated PTSD can lead to maladaptive coping or chronic issues into adulthood.
How can I tell the difference between normal teen behavior and PTSD symptoms?
PTSD differs in timing, intensity, and context. Symptoms are consistent, linked to trauma, and cause sudden changes across behavior, mood, and functioning. Normal teen moodiness fluctuates naturally, with gradual shifts in interests and social connections, rather than abrupt disruption.
Can trauma experienced in childhood show up as PTSD years later in the teen years?
Yes. Delayed-onset PTSD can emerge months or years later, often during adolescence due to developmental changes, social pressures, or triggers echoing the original trauma. Adolescents’ growing cognitive skills can make previously unprocessed trauma fully recognized, activating symptoms.
How can I support my daughter without becoming overprotective?
Balance safety and independence. Use protective measures that genuinely reduce risk, collaborate with her and her treatment team, and allow gradual exposure to manageable fears. Open communication and flexible support help restore autonomy and encourage healthy coping.
Can teens fully recover from PTSD?
With proper treatment and support, most teen girls experience significant recovery. Programs those at like Mission Prep provide guidance, coping strategies, and structured support, helping teens use adolescent brain plasticity to heal, build resilience, and thrive beyond their trauma.