Key Takeaways
- Anorexia nervosa is one of the deadliest mental health conditions, with affected individuals having up to five times the mortality risk of the general population.
- Early warning signs include not only weight loss but also behavioral changes such as food rituals, social withdrawal, and obsessive exercise patterns.
- The most effective treatment approaches involve multidisciplinary care teams and family-based therapy, with early intervention significantly improving recovery outcomes.
- Creating a supportive home environment that separates the teen from the disorder is crucial for successful recovery.
- Mission Prep Healthcare provides comprehensive care for eating disorders by addressing underlying mental health conditions such as anxiety, depression, and trauma through therapies like mindfulness-based CBT and somatic approaches to support lasting recovery.
The Silent Epidemic: How Anorexia Affects Teen Girls Today
Anorexia nervosa is characterized by severe calorie restriction, intense fear of weight gain, and distorted body image. It represents much more than just “extreme dieting”—it’s a serious psychiatric condition that can devastate physical health and emotional well-being.
For teenagers, whose bodies are still developing, the consequences can be particularly severe, affecting everything from bone density to brain development. The disorder typically emerges during adolescence, a time of significant physical and emotional changes.
Social media platforms filled with idealized body images, peer pressure, and the developmental search for identity all create perfect conditions for eating disorders to take root. What often begins as seemingly innocent dietary changes can quickly spiral into obsessive behaviors and dangerous health complications.
Why Teen Girls Are Particularly Vulnerable
Adolescent girls face unique pressures that make them especially susceptible to anorexia nervosa. Puberty brings significant body changes that can feel overwhelming and beyond their control.
For many girls, food restriction becomes a misguided attempt to manage anxiety and establish a sense of control during this tumultuous developmental period.
Social media compounds these vulnerabilities by constantly exposing teens to unrealistic beauty standards and promoting “wellness” content that often glorifies extreme thinness under the guise of health.
The Life-Threatening Reality of Untreated Cases
Untreated anorexia can lead to severe medical complications, including heart problems, bone density loss, and multi-organ failure. The cardiovascular system becomes particularly compromised as the body begins to break down muscle tissue, including heart muscle, for energy.
Electrolyte imbalances can cause dangerous heart rhythm disturbances, while hormonal disruptions halt menstruation and impair fertility. Cognitive function declines as the brain is deprived of essential nutrients, leading to difficulties with concentration, decision-making, and emotional regulation.
These physiological changes create a dangerous cycle where rational thinking becomes increasingly impaired, making it harder for the teenager to recognize the severity of their condition or accept help.
Mission Prep Healthcare specializes in mental health treatment for teens aged 12-17, offering residential and outpatient programs for anxiety, depression, trauma, and mood disorders. Our therapies include CBT, DBT, EMDR, and TMS, tailored to each adolescent’s needs.
With a structured, supportive environment, we integrate academic support and family involvement to promote lasting recovery. Our goal is to help teens build resilience and regain confidence in their future.
4 Warning Signs of Anorexia Every Teen Should Know
Recognizing anorexia early requires looking beyond apparent weight loss to subtle behavioral and emotional changes.
Physical Changes Beyond Weight Loss
The physical signs of anorexia nervosa extend far beyond simply becoming thin. Teens should watch for fine, downy hair (lanugo) on the body, which is the body’s attempt to keep warm as it loses insulating fat.
Brittle nails, thinning hair, and dry skin often develop as the body diverts limited nutrients to vital organs. Constant complaints of feeling cold, even in warm environments, signal that the body has lost its natural insulation and ability to regulate temperature properly.
Dental problems might emerge as stomach acid damages tooth enamel from frequent vomiting if purging behaviors are present. Menstrual cycles typically become irregular or stop altogether (amenorrhea) as the body conserves energy by shutting down reproductive functions.
These physiological changes often progress gradually, making them easy to miss unless parents are specifically looking for them.
Behavioral Red Flags Around Meals
Food rituals offer critical clues to developing anorexia. Teens might suddenly develop an intense interest in cooking elaborate meals for others while barely eating themselves. Cutting food into tiny pieces, moving food around the plate without eating it, and developing rigid rules about “safe” and “unsafe” foods are common behaviors.
Many teens with anorexia create elaborate excuses to avoid family meals, claiming they’ve already eaten elsewhere or have stomach pain that prevents eating.
Obsessive calorie counting, researching the nutritional content of everything, or refusing to eat anything without knowing its exact ingredients are additional warning signs.
Teens with anorexia develop a preoccupation with food—talking about it constantly, collecting recipes, watching cooking shows—while paradoxically restricting their own intake more severely.
Emotional & Social Withdrawal Patterns
As anorexia strengthens its grip, teens often withdraw from social activities, particularly those involving food. Birthday parties, family gatherings, and restaurant outings become sources of anxiety rather than joy.
Friends may report that your teen has become isolated or obsessed with appearance and weight. Irritability, depression, and anxiety frequently accompany anorexia as both symptoms and contributing factors to the disorder’s development.
Academic performance may improve as teens channel perfectionistic tendencies into schoolwork, but concentration eventually suffers as malnutrition affects brain function. Sleep disturbances are also common, with many teens experiencing insomnia or restless sleep patterns.
Exercise Obsession & Body Checking
Excessive exercise that feels compulsive rather than enjoyable represents a major red flag for anorexia. Teens might exercise despite injury, illness, or extreme weather conditions, feeling intense guilt or anxiety if they miss a workout.
They often exercise in private, sometimes performing countless repetitions of simple exercises like sit-ups or push-ups in their bedroom late at night. Constant body checking behaviors can signal unhealthy body image concerns. These may include repeatedly examining specific body parts in mirrors, measuring body parts with fingers or tape measures, or seeking reassurance about appearance.
Many teens with anorexia wear oversized clothing to hide their bodies, not out of modesty but to conceal weight loss from concerned adults. Some develop a distorted perception where they genuinely see themselves as overweight despite being dangerously thin – a phenomenon called body dysmorphia that often accompanies anorexia.
Treatment Approaches That Actually Work
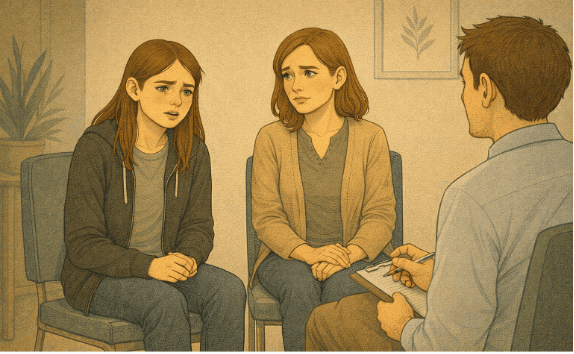
Effective treatment for anorexia nervosa requires a comprehensive approach that addresses both physical restoration and the psychological aspects of the disorder.
The Multi-Disciplinary Team Teens Need
Recovery from anorexia requires a coordinated team of specialists working together to address the complex physical and psychological aspects of the disorder.
At the center of this team is typically a child/adolescent psychiatrist or psychologist who specializes in eating disorders and can oversee the overall treatment plan. Other team members who ensure all-around recovery include:
- Pediatrician or adolescent medicine physician for medical monitoring
- Registered dietitian with eating disorder expertise
- Psychiatric nurse or case manager
- Family therapist (often critical for family-based treatment approaches)
These mental health professionals bring specific training in the cognitive and emotional patterns that maintain anorexia, helping teens challenge distorted thoughts about food, weight, and body image.
Family-Based Treatment: The Gold Standard
Family-Based Treatment (FBT), also called the Maudsley Approach, represents the most evidence-based intervention for adolescent anorexia. This approach radically repositions parents as the primary agents of recovery rather than viewing them as part of the problem.
Parents temporarily take complete control of meals and nutrition, providing the consistent structure needed to overcome the powerful grip of anorexia on your teen’s eating behaviors.
In the first phase of FBT, parents work with the treatment team to develop and implement a plan for weight restoration, learning specific techniques for managing meal-related anxiety and resistance.
The family therapist helps parents present a united front against the disorder while supporting their child’s emotional needs. Siblings are included in treatment discussions to help them understand their role in supporting recovery while maintaining their own emotional well-being.
When Hospitalization Becomes Necessary
Inpatient treatment becomes necessary when medical complications reach life-threatening levels or when outpatient approaches haven’t produced sufficient progress.
Warning signs that hospitalization may be needed include a heart rate below 50 beats per minute, changes in blood pressure upon standing (orthostatic hypotension), a body temperature below 96°F, severe electrolyte imbalances, or rapid weight loss exceeding 15%–20% of healthy body weight.
Hospital programs provide 24-hour medical monitoring, structured meal support, and intensive therapy in a controlled environment, allowing nutritional rehabilitation to proceed safely.
For many teenagers, this level of care serves as a crucial stabilization period before transitioning to intensive outpatient or partial hospitalization programs that bridge the gap between inpatient and regular outpatient care.
3 Crucial Ways Parents Can Support Recovery
1. Create a Safe Food Environment at Home
Restructuring your home food environment is essential when supporting a teen with anorexia. Remove diet products, calorie-counting apps, and scales that can trigger obsessive behaviors.
Instead, stock your kitchen with a variety of nutritious foods that support recovery, including those that might initially cause anxiety for your teen. Having regular, planned meals and snacks creates predictability that helps reduce mealtime anxiety.
2. Separate Your Child from the Disorder
One of the most potent approaches in supporting recovery is learning to view anorexia as separate from your child. When you can recognize that the hurtful behaviors, resistance to treatment, and food-related anxiety come from the disorder rather than your child’s true self, it becomes easier to remain compassionate.
This perspective allows you to ally with your teen against the eating disorder instead of battling each other. Try using language that externalizes the disorder, such as “I know the eating disorder is making you afraid of this food,” rather than “Why won’t you just eat?”
3. Model Healthy Attitudes About Food & Bodies
Parents are powerful influences on how children perceive food and body image, even during the teenage years when peer influence increases. Examine your own relationship with food, weight, and body image, being mindful of comments about your appearance or others’.
Avoid diet talk, negative body comments, or expressions of guilt about eating certain foods. Instead, model balanced eating that emphasizes nourishment and enjoyment rather than restriction or control. Show comfort with normal body diversity and appreciation for what bodies can do rather than how they look.
Start Your Teen’s Recovery Journey at Mission Prep
Anorexia nervosa is a complex, life-threatening condition that requires swift, compassionate intervention. Recognizing the warning signs from food rituals and social withdrawal to obsessive exercise and body image distortion is the first step toward getting the help you need. With evidence-based treatments and a dedicated multidisciplinary team, recovery is absolutely possible.

Visit Mission Prep to discover how we can help your family find hope again.
At Mission Prep, we understand that eating disorders rarely exist in isolation. While we don’t treat eating disorders directly, we specialize in addressing the underlying mental health conditions, anxiety, depression, and trauma that often fuel disordered eating.
Through mindfulness-based CBT, art therapy, and somatic therapies, we help teens develop healthier coping mechanisms and build emotional resilience essential for lasting recovery.
Frequently Asked Questions (FAQs)
What are the first warning signs of anorexia nervosa in teenage girls?
Early signs include developing rigid food rules, making excuses to skip meals, and an intense interest in cooking while barely eating. Physical signs include persistent coldness, thinning hair, and menstrual irregularities. Social withdrawal and increased anxiety around mealtimes also warrant professional evaluation.
How is anorexia nervosa different from regular teenage dieting?
The key distinction is rigidity and emotional distress. While typical dieting involves flexible goals, anorexia creates increasingly restrictive rules regardless of physical consequences. When eating triggers intense anxiety or guilt, or when body checking becomes compulsive, these responses signal something more serious.
What does effective treatment for teenage anorexia look like?
Effective treatment requires a multidisciplinary team including a psychiatrist, pediatrician, dietitian, and family therapist. FBT is considered the gold standard, where parents temporarily take control of meals while therapists coach them through the recovery process.
How can parents support their teenager’s recovery at home?
Create a safe food environment free of diet products and scales, establish consistent mealtimes, and avoid labeling foods as “good” or “bad.” Separate your child from the disorder, remain calm during meals, and model healthy attitudes about food and bodies.
Does Mission Prep treat eating disorders in teenagers?
Mission Prep doesn’t treat eating disorders directly but provides support by addressing underlying conditions like trauma, anxiety, and depression. Through mindfulness-based CBT, art therapy, and somatic therapies, we help teens build emotional resilience essential for lasting recovery.