Skin Picking in Teens: Causes, Signs, and Support Strategies

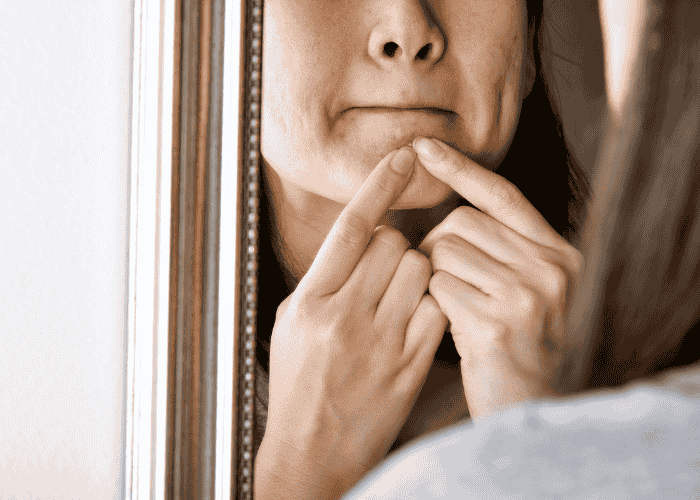
So, for many parents, skin picking in teens doesn’t raise alarm bells at first. But over time, you may start to notice signs, such as your teen scratching their face while watching TV, or covering up small wounds with makeup or band-aids.
When it first starts to happen, it’s easy to chalk it up to just being a phase. But when picking becomes repetitive, hard to stop, and starts leaving marks or wounds, it may be more than a habit. It may be a clinical condition called skin picking disorder, a type of body-focused repetitive behavior (BFRB) related to obsessive-compulsive tendencies.1,2
The earlier the skin picking disorder is noticed, the easier it is to find the right support and for teens to recover.1 So, this article covers:
What skin picking disorder is- Symptoms of adolescent dermatillomania
- Risk factors and causes of skin picking in teens
- Treatment for teen skin picking disorder
- Coping strategies for body-focused behaviors in adolescents
- Parental support for dermatillomania
What Is Skin Picking Disorder in Teens?
The usual focal points of picking are:4
Arms, including your hands, fingers, and forearms- Head, such as your neck, face, and scalp
- Legs, including your feet, toes, calves, or thighs
Skin picking disorder typically begins during the teen years, often aligning with the start of puberty (13-15 years), and tends to affect around 1-5% of the population.5
When you see your teen picking their skin, it’s easy to assume they’re choosing to do so. It may be frustrating as a parent if you’ve told them to stop and yet they continue to pick, even to the point of pain. It’s important to know that clinically, dermatillomania is recognized in the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5) as an obsessive-compulsive–related disorder.6 So, know that skin picking disorder isn’t a choice – it’s a mental health condition. And your teen may feel just as negatively towards it as you do.
Symptoms of Adolescent Dermatillomania
We may all pick our skin at times, especially if we notice a pimple or bump. However, what distinguishes normal picking from skin picking disorder is:
Being unable to stop picking at your skin- Causing skin damage, such as bleeding, bruising, or cuts, as a result of picking
- Trying to remove or smooth “imperfections” such as bumps, spots, or moles
- Picking at your skin without realizing you’re doing it
- Picking your skin when you’re feeling stressed or anxious
- Extended time spent picking, sometimes for hours, in private
- Emotional distress after picking, such as guilt, frustration, or sadness
Not all teens will show every symptom, but these patterns often signal when skin picking has become more than a habit.7 Because teens often struggle silently, these signs may be subtle at first. However, getting to grips with the signs is important as early recognition gives the best chance for recovery without long-term effects.7
Risk Factors and Causes of Skin Picking in Teens
This isn’t the only factor that puts people at risk of developing skin picking disorder. Dermatillomania rarely has a single cause. Instead, it usually develops through a mix of emotional, biological, and environmental influences.8 Breaking the cycle of picking requires understanding all of the potential factors at play.1,9
Psychological and Emotional Influences
Stress, anxiety, or obsessive thinking- Perfectionism or hyper-focus on perceived flaws
- Trauma or emotionally overwhelming situations
Emotional Triggers
Boredom, loneliness, or sadness- Moments of rest or inactivity, like watching TV or lying in bed, as picking can become a form of stimulation
- Picking as a form of self-soothing or escape
Biological and Genetic Factors
Imbalances in serotonin or dopamine regulation.1- Family history of OCD, anxiety, or BFRBs
Environmental Influences
Stress and high pressure from school, sports, or family expectations- Lack of alternative coping strategies
Today’s teens face many pressures, which may contribute to skin picking. Social media focuses heavily on appearance and can even make small blemishes like acne feel unbearable to a teen.9 Academia is also often a source of stress, as is the demand to participate in sports or other groups and clubs outside of school. Finally, puberty comes with a huge shift in hormones and causes bodily changes, all of which can take a toll on a teen’s well-being.
When it comes to skin picking, none of these factors acts alone. But in unison, they can trigger heightened stress levels, which may push teens closer to unhealthy coping strategies like skin picking.12
Co-Occurring Conditions
Alongside the factors we mentioned above, teens may struggle with mental health conditions that put them at higher risk of experiencing skin picking disorder. For example, teens with ADHD, depression, generalized anxiety, or other compulsive behaviors have a higher likelihood of developing dermatillomania.8
Treatment for Teen Skin Picking Disorder
Evidence-Based Therapies
Cognitive Behavioral Therapy (CBT): CBT helps teens understand the thoughts and feelings that lead to picking and helps them learn healthier coping strategies.13- Habit Reversal Training (HRT): HRT teaches teens to replace picking with healthier physical actions (like squeezing a stress ball or clenching fists).14
- Acceptance and Commitment Therapy (ACT): A few studies also suggest that ACT can help teens who are struggling with skin picking disorder. However, more research is needed to confirm this.15
Medication Support
There are no medications specific to skin picking disorder. However, in some cases, doctors may prescribe SSRIs (selective serotonin reuptake inhibitors) for SPD, especially when anxiety or OCD symptoms are strongly present.3
The sooner treatment begins, the easier it is to prevent long-term skin damage and the potential emotional consequences of this condition.7
When considering the treatment options for a teen with skin picking disorder, it’s important to remember that treatment will likely not be a quick fix. Progress is gradual and happens one step at a time. In therapy, it begins with tracking the urges and documenting the times and situations that trigger skin picking behaviors. Then replacement habits and healthier coping strategies need to be built, which takes time.2
What’s more, relapse can happen. If you find your teen picking their skin again, this does not mean they’ve ‘failed’ – it’s part of the learning process. The overall goal is to help symptoms lessen over time and build hope that the teen can handle the urges in a healthier way.
Coping Strategies for Body-Focused Behaviors in Adolescents
- Mindfulness practices, including breathing exercises, journaling, or grounding techniques, can help regulate stress.
- Fidget alternatives, such as textured fabrics, putty, or handheld gadgets to redirect the hands.
- Structured routines, including reducing idle time, as this lowers opportunities to pick.
- Practicing healthy skin care, like using moisturizers or acne treatments, may reduce sensations that trigger picking.
- Confidence-building activities, such as engaging in hobbies, sports, or creative outlets, can improve a teen’s mood and sense of self-image.
Healing doesn’t come from forcing the behavior to stop. It comes from replacing the behavior with healthier habits.
Parental Support for Dermatillomania: How to Help
- Staying calm and avoiding blame
- Treating it as a health issue, not defiance
- Encouraging therapy early, without making it feel like punishment
- Working together to identify stress triggers
- Modeling healthy coping habits in the household
- Celebrating small wins, rather than focusing on setbacks.
When teens feel seen, they are far more likely to accept help and heal.
Just as important is what parents need to avoid. We recommend avoiding criticizing, scolding, or comparing a teen to others. This can worsen the shame that a teen may feel around their skin picking and can make the behavior worse.
Instead, approach the situation with curiosity and patience. Let your teen know that you see them and you see their struggle. Help them realize their own strength. This combination of empathy and belief in them can support them to develop the skills needed to reduce their skin picking behaviors.
When It’s Time to Seek Professional Help
If your teen’s skin picking has reached the point where it’s leaving damage or interfering with their daily life, we recommend reaching out to a mental health professional.
At Mission Prep, treatment isn’t one-size-fits-all. Everyone has a unique story. That’s why our programs use evidence-based therapy (like CBT and habit reversal training) that meet teens right where they are.
We know that when one teen struggles, it affects the entire family. That’s why we involve parents in the process; not only to understand what’s happening, but to give parents the tools and strategies to walk alongside their child in their mental health healing journey.
Mission Prep provides both a safe space and guidance to make recovery possible. Whether that be outpatient services, tailored to fit around a teen’s school life, or a residential program for those in need of more structured support.

Mission Prep: Therapeutic Support for Skin Picking Disorder
Skin picking may feel isolating for both teens and parents, but it doesn’t have to stay that way. With the right support, skin picking behaviors can be a thing of the past.
If you’re noticing skin picking or mental health difficulties in your teen, reach out to Mission Prep today. Together, we can help your teen break free from skin picking and step into a healthier, more confident future.
References
- Grant, J. E., Odlaug, B. L., Chamberlain, S. R., Keuthen, N. J., Lochner, C., & Stein, D. J. (2012b). Skin picking disorder. American Journal of Psychiatry, 169(11), 1143–1149. https://doi.org/10.1176/appi.ajp.2012.12040508
- Lochner, C., Roos, A., & Stein, D. (2017). Excoriation (skin-picking) disorder: a systematic review of treatment options. Neuropsychiatric Disease and Treatment, Volume 13, 1867–1872. https://doi.org/10.2147/ndt.s121138
- NHS. (2025, May 2). Skin Picking Disorder. https://www.nhs.uk/mental-health/conditions/skin-picking-disorder/
- Cleveland Clinic. (2025, June 2). Dermatillomania (Skin picking). https://my.clevelandclinic.org/health/diseases/22706-dermatillomania-skin-picking
- Mental Health America. (2025, September 26). Excoriation Disorder (Skin picking or dermatillomania). https://mhanational.org/conditions/excoriation-disorder-skin-picking-or-dermatillomania/
- Substance Abuse and Mental Health Services Administration. (2016). Impact of the DSM-IV to DSM-5 Changes on the National Survey on Drug Use and Health. https://www.ncbi.nlm.nih.gov/books/NBK519704/table/ch3.t28/
- Eskeland, S. O., Moen, E., Meland, K. J., Andersen, A., & Hummelen, B. (2021). Hudplukkingslidelse. Tidsskrift for Den Norske Legeforening. https://doi.org/10.4045/tidsskr.21.0128
- Odlaug, B. L., & Grant, J. E. (2008). Clinical characteristics and medical complications of pathologic skin picking. General Hospital Psychiatry, 30(1), 61–66. https://doi.org/10.1016/j.genhosppsych.2007.07.009
- Gallinat, C., Stürmlinger, L. L., Schaber, S., & Bauer, S. (2021). Pathological skin picking: phenomenology and associations with emotions, Self-Esteem, body image, and Subjective Physical Well-Being. Frontiers in Psychiatry, 12. https://doi.org/10.3389/fpsyt.2021.732717
- Smith, A. J. (2024, April 1st). How to stop pulling or picking. Anxiety & Depression Association of America. https://adaa.org/learn-from-us/from-the-experts/blog-posts/consumer/how-stop-pulling-or-picking
- Schienle, A., & Wabnegger, A. (2020). Two subtypes of pathological skin-picking: Evidence from a voxel-based morphometry study. Journal of Obsessive-Compulsive and Related Disorders, 25, 100534. https://doi.org/10.1016/j.jocrd.2020.100534
- Garey, J. (n.d.). What is excoriation, or skin-picking? Child Mind Institute. https://childmind.org/article/excoriation-or-skin-picking/
- Revankar, R. R., Revankar, N. R., Balogh, E. A., Patel, H. A., Kaplan, S. G., & Feldman, S. R. (2022). Cognitive behavior therapy as dermatological treatment: A narrative review. International Journal of Women’s Dermatology, 8(4), e068. https://doi.org/10.1097/JW9.0000000000000068
- Batchelor, R., Penn, C., & Anderson, C. (2024). Cognitive behavioural therapy including habit reversal training for treating dermatillomania in the context of anxiety and low mood. The Cognitive Behaviour Therapist, 17, e17. https://doi.org/10.1017/S1754470X24000163
- Twohig, M. P., Hayes, S. C., & Masuda, A. (2006). A preliminary investigation of acceptance and commitment therapy as a treatment for chronic skin picking. Behaviour research and therapy, 44(10), 1513–1522. https://doi.org/10.1016/j.brat.2005.10.002













